[ENDOSTORY #2] From “Gastritis” to Early Gastric Cancer – The Power of Magnifying Endoscopy Combined with NBI
A 65‑year-old female patient, initially diagnosed with hemorrhagic gastritis in the gastric antrum at a local clinic and unresponsive to a course of medication, presented at K Hospital’s Quán Sứ branch for a screening endoscopy.
Upon repeat endoscopic examination, the physician diagnosed Early Gastric Cancer (EGC). How could an actual early-stage malignancy be mistaken for simple gastritis? And how can such misdiagnoses or oversights—leading to loss of the “golden window” for cancer treatment—be prevented? This article reviews the endoscopic images and provides rational criteria to accurately assess lesion nature in early cancer diagnosis and management.
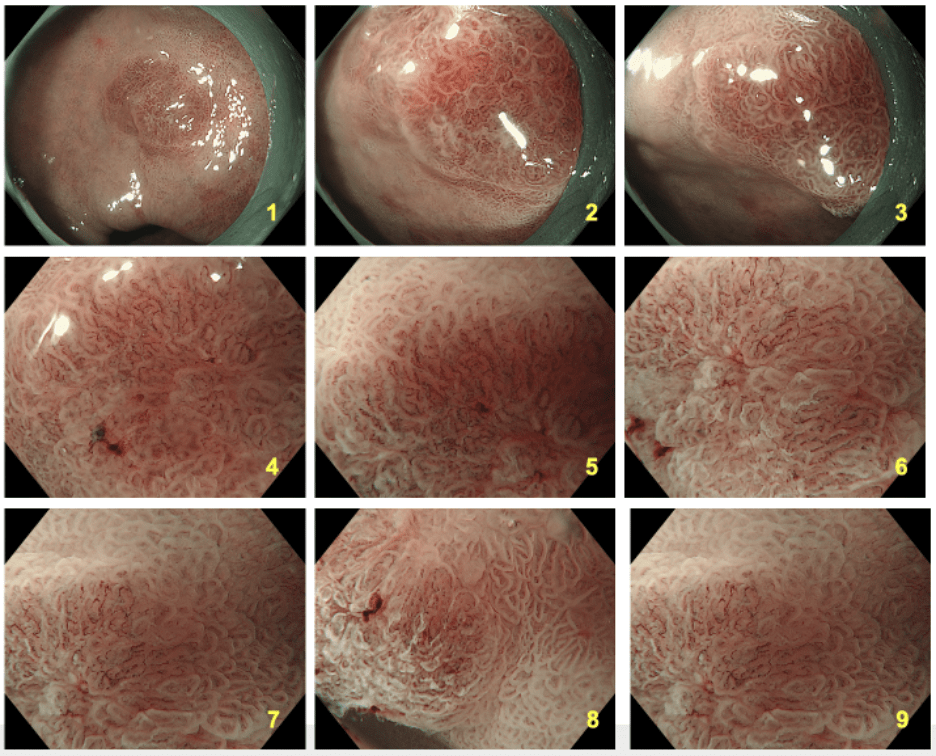
White-Light Imaging (WLI) Findings
Under WLI, a subtle, slightly elevated, non-pedunculated red lesion with blurred margins was observed on the lesser curvature of the antrum, easily overlooked at a glance. This is a nonpolypoid lesion (Paris classification 0-IIa)—a typical presentation of early gastric cancer but notoriously difficult to detect under WLI alone.
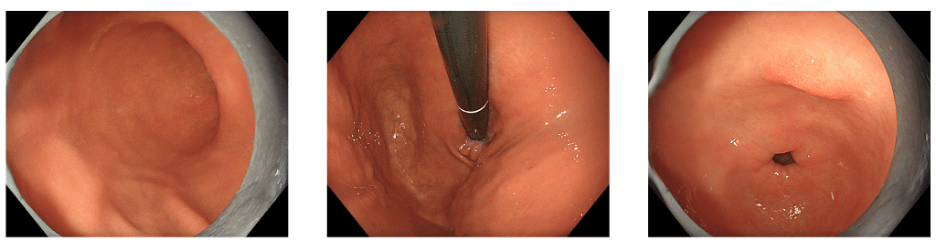
Because of its subtle appearance, the lesion was initially overlooked, resulting in inappropriate treatment. Compared to benign lesions—such as polyps (pedunculated, protruding, bright red, with clear boundaries) or widespread erosive gastritis (extensive inflammation and hyperemia)—this lesion was solitary, slightly raised, and localized. However, WLI alone was insufficient to unveil its true nature, necessitating further assessment with magnifying endoscopy combined with NBI (M‑NBI).
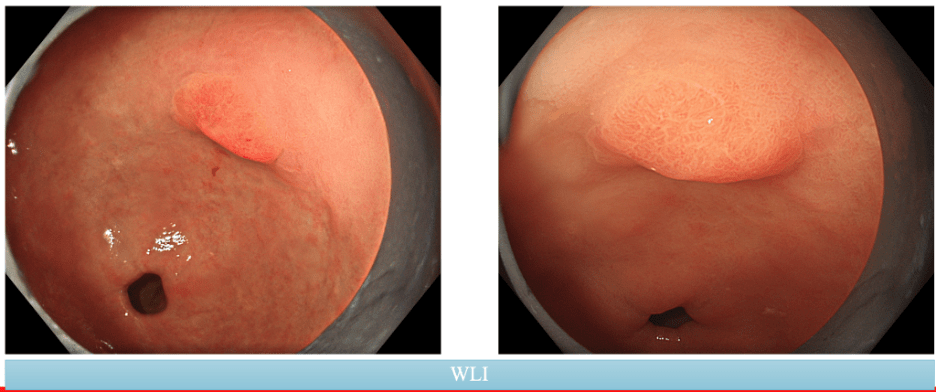
Magnifying Endoscopy + NBI for Lesion Characterization: Always Observe from Multiple Angles for Accurate Assessment
While WLI gives a general overview, Magnifying Endoscopy combined with NBI (M‑NBI) is the true key to identifying lesion nature. It provides a clear view of both the microvascular architecture (MV) and the microsurface structure (MS) of the lesion.
M‑NBI is an endoscopic technique that combines image magnification (magnifying endoscopy) with Narrow-Band Imaging, enhancing the contrast of microvascular and mucosal surface structures. This technology utilizes blue light (wavelengths 415 nm and 540 nm), which is strongly absorbed by hemoglobin, highlighting superficial subepithelial vessels, while the magnification allows clear visualization of each glandular pit, epithelial pit borders, and capillaries.
VSCS Classification System: A “Map” to Read M‑NBI Images
Having understood M‑NBI’s function, the vital question is: how do we interpret the acquired images objectively and systematically? That is why the Vessel plus Surface Classification System (VSCS) was developed—considered a “gold standard” endorsed by many endoscopy associations for evaluating gastric lesions with magnifying NBI.
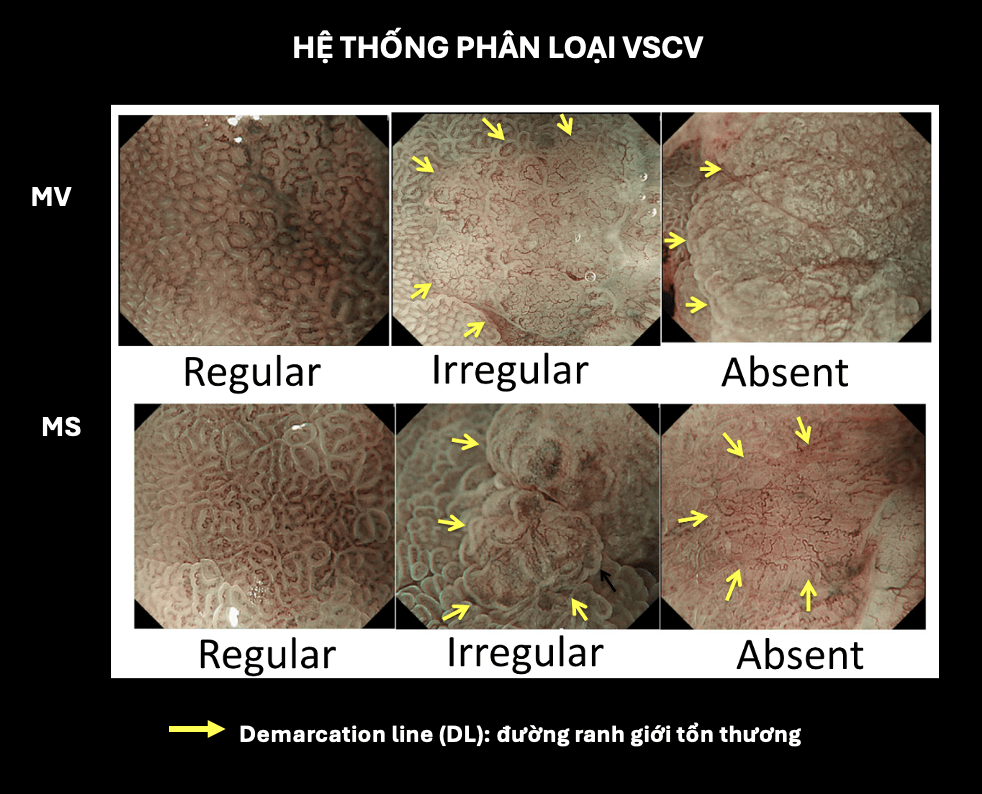
VSCS analyzes two principal microscopic features of the mucosa under M‑NBI:
- Microvascular architecture (MV)
- Microsurface structure (MS)
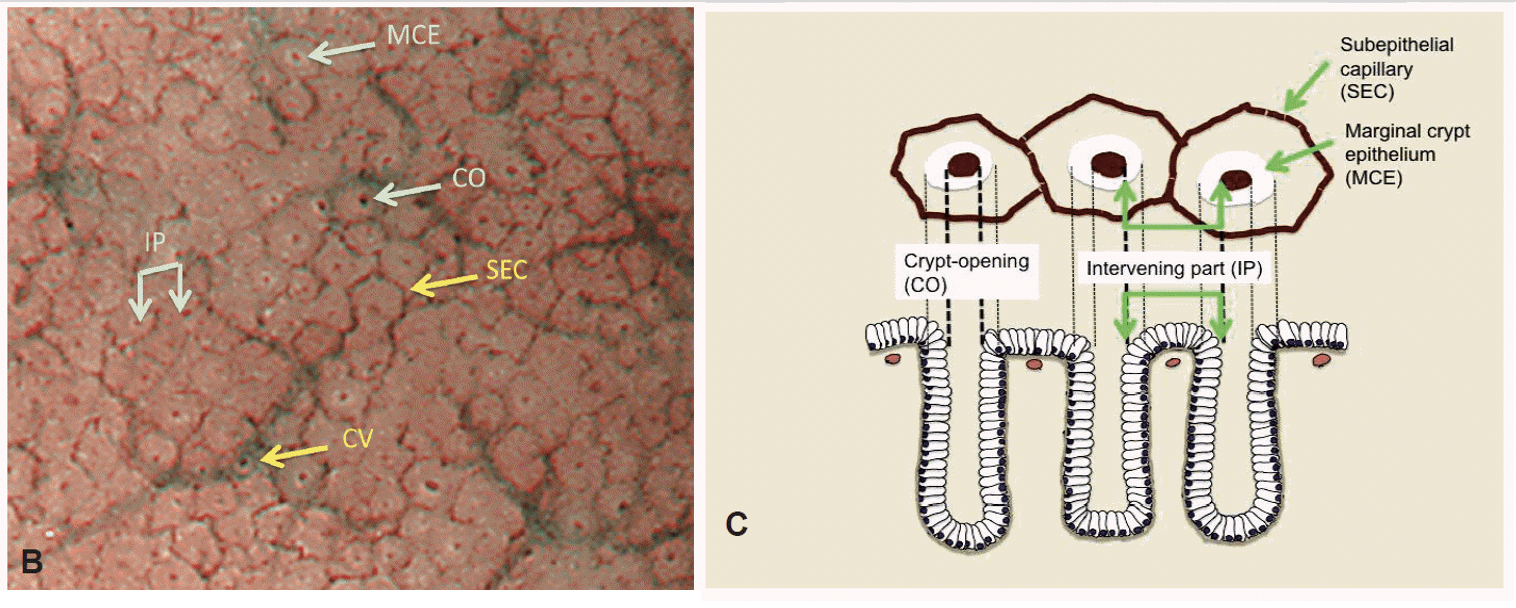
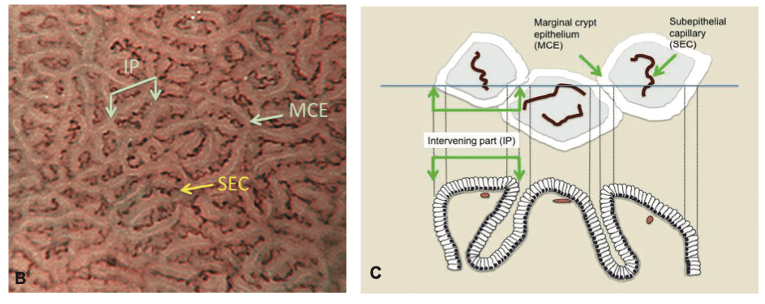
In normal mucosa, these features have distinct patterns depending on anatomical location:
- Gastric fundic mucosa: a regular subepithelial capillary network (SEC) in a honeycomb pattern, clear capillary vasculature (CV); gland pits are round and uniform, with clearly defined epithelial pit borders.
- Pyloric mucosa: SEC in a spiral pattern; CV absent; surface structure forms arches or polygon shapes arranged symmetrically.
Based on these norms, VSCS classifies MV and MS into three states: regular, irregular, and absent:
| Feature | Regular | Irregular | Absent |
| MV | Subepithelial capillaries (SECs) have a uniform shape, which may be either closed loops (polygonal shapes) or open loops, with consistent morphology, symmetrical distribution, and an orderly arrangement. | Blood vessels may appear as closed loops (polygonal), open loops, tortuous, branched, or irregular in shape, with or without a network-like pattern. They exhibit heterogeneous morphology, asymmetrical distribution, and a disorganized arrangement. | Not observable due to being obscured by a white opaque substance (WOS – White Opaque Substance). |
| MS | The marginal crypt epithelium (MCE) appears uniform, with a linear or round shape, clearly defined borders, and a regularly arranged pattern. | MCE may appear linear, curved, oval, round, or villous with heterogeneous morphology, asymmetrical distribution, and irregular arrangement. | Both MCE and WOS are not visible on the M-NBI image. |
MESDA‑G: A Fast Diagnostic Algorithm
After evaluating mucosal microstructure using VSCS, a more clinically oriented method is required to decide whether a lesion is compatible with early gastric cancer. That is the purpose of MESDA‑G (Magnifying Endoscopy Simple Diagnostic Algorithm for Gastric cancer)—a fast, simple, highly accurate diagnostic algorithm especially designed for magnifying endoscopy.
MESDA‑G is implemented in two steps:
1. Check for a Demarcation Line (DL):
- No DL → benign lesion
- DL present → proceed to step 2
2. Assess MV and MS
- If either MV or MS is irregular → high likelihood of malignancy
- If MV and MS are both regular or both absent → likely benign
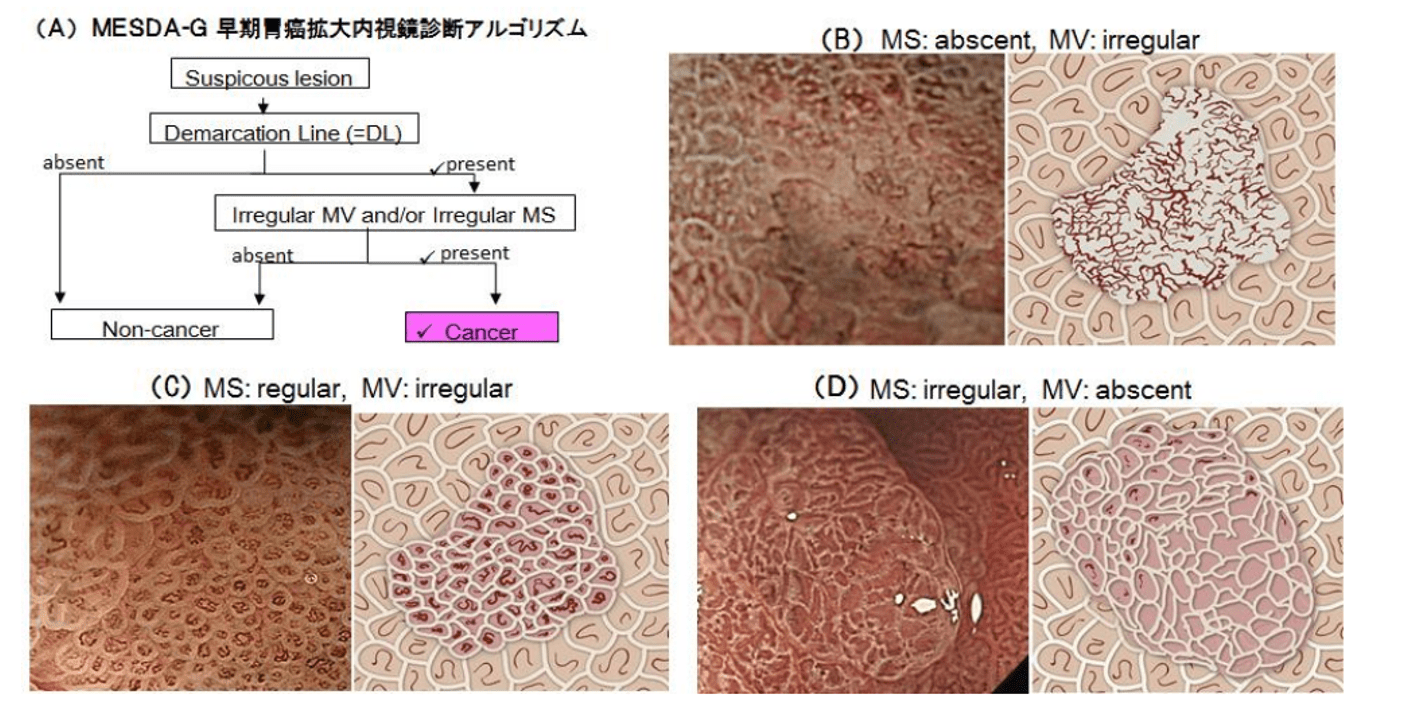
Applying MESDA‑G in this case, we can conclude early cancer characteristics:
- A clear demarcation line (DL)
- Irregular microvascular architecture (MV): abnormal open-loop vessels, dilation, heterogeneous morphology, uneven distribution
- Irregular microsurface structure (MS): MCE with multiple, heterogeneous shapes
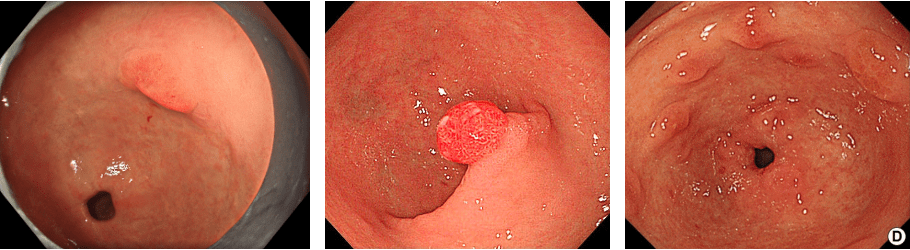
Final Diagnosis and Treatment Outcomes
Upon completing upper GI endoscopy and evaluating the suspicious lesion in the antrum using WLI and M‑NBI:
- Location: lesser curvature of the antrum (L – Lesser curvature)
- Macroscopically: slightly elevated (Paris classification: 0‑IIa)
- Lesion size: 10 × 8 mm
Initial diagnosis:
- Early Gastric Cancer (EGC)
- Predicted invasion depth: Tis – T1a
- Treatment indication: Absolute indication for ESD
Histopathology after ESD:
- Moderate differentiated tubular adenocarcinoma (tub1)
- Depth of invasion: pTis – confined to mucosa
- No vascular or lymphatic invasion: ly0, v0
- Negative resection margins: HM0 (horizontal), VM0 (vertical)
In addition, surrounding mucosa exhibited chronic inflammation and intestinal metaplasia, but no evidence of cancer at the resection margins.
Lesson from This Case: Don’t Let Early Gastric Cancer Be Missed
This case is a clear testament to the power of magnifying endoscopy with NBI (M‑NBI) in detecting and evaluating early gastric cancer lesions that may be mistaken for gastritis or benign polyps.
Using tools like the Paris classification, VSCS, and MESDA‑G, physicians were able to:
- Detect atypical lesions in difficult-to-observe locations.
- Accurately differentiate malignant lesions from benign inflammation.
- Make correct decisions about ESD indication and avoid unnecessary surgery.
Timely detection and treatment allowed the patient to avoid progression to advanced-stage gastric cancer and preserve optimal quality of life.
Reference:
Kenshi Yao – Clinical Application of Magnifying Endoscopy with Narrow‑Band Imaging in the Stomach
About ENDOSTORY
ENDOSTORY is a clinical case-sharing series in gastrointestinal endoscopy presented by Lenus Vietnam, aiming to provide practical and useful information for endoscopists. Each week, one “story” is selected and posted on the Lenus Vietnam Facebook page at 8 PM every Friday.
The series is medically supervised by Dr. Trần Cảnh—a specialist in early cancer diagnosis and treatment. Not only has Dr. Cảnh personally participated in many complex ESD cases, but he has also trained numerous young Vietnamese endoscopists in ESD, contributing to the widespread adoption of this “golden key” technique in early gastrointestinal oncology. His spirit of sharing inspired the ENDOSTORY storytelling initiative.
This program is still in its early stages and greatly welcomes feedback for improvement.
For any feedback or inquiries, please send a message via the Lenus Vietnam Facebook fanpage or email [email protected]—we’d be delighted to hear from you.