NBI-Assisted Endoscopy – A “Visual Weapon” Elevating Diagnostic and Therapeutic Endoscopy
Before the advent of NBI technology, white-light imaging was the most advanced observation mode endoscopists could rely on to assess the mucosa of the gastrointestinal (GI) tract. Despite being the primary observation mode, white light has significant limitations, especially when dealing with small, flat, or color-similar lesions. Early detection, lesion characterization, and real-time treatment decision-making have always been clinical challenges. From this need, advanced image-enhancement technologies emerged, among which Narrow Band Imaging (NBI)—an optical enhancement technology developed by Olympus and first introduced in 2005—stands out.
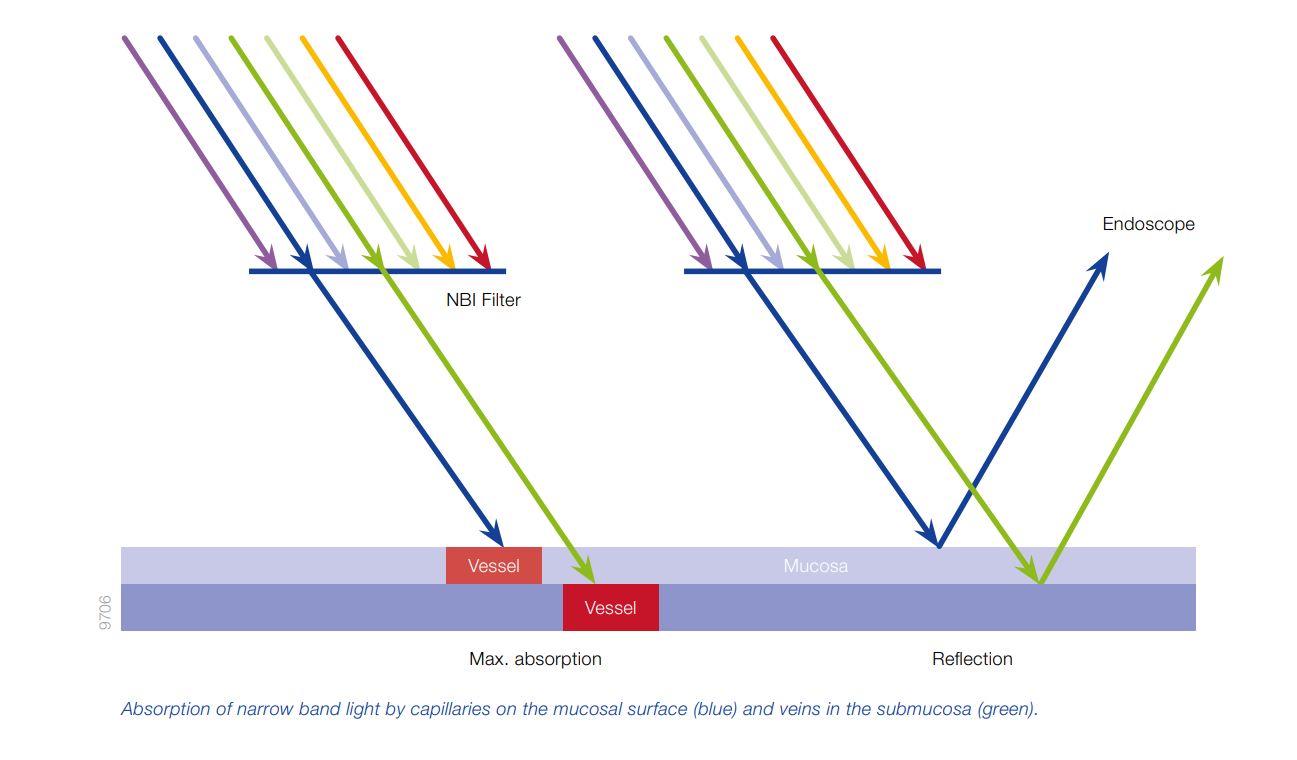
Narrow Band Imaging (NBI) is an optical image enhancement technology that significantly improves the visualization of mucosal surface structures and microvasculature. The technology works based on light wavelength selection. Human-visible light only accounts for a small portion of the electromagnetic spectrum. When light hits an object, part of it is absorbed and the rest is reflected—the reflected light determines the color we see. In white-light endoscopy (WLE), the light source emits a broad range of wavelengths, which can result in images with low contrast when detecting subtle abnormalities. NBI, on the other hand, uses a special narrow-band filter that only allows two wavelengths to pass through: blue light (415 nm) and green light (540 nm). These wavelengths correspond to the absorption peaks of hemoglobin (a protein in red blood cells), allowing strong absorption by superficial capillaries under the mucosa. As a result, NBI highlights the vascular structures and mucosal microarchitecture, helping clinicians detect subtle lesions that standard white light may miss.
How Does NBI Support Clinical Endoscopy, Especially in Early Cancer Detection?
Seeing What White Light Cannot: Detecting Early Lesions and Unlocking Life-Saving Opportunities
Early-stage lesions often appear in various forms—flat, depressed, granular, or small—and are nearly “hidden” beneath the mucosa, making them difficult to detect with white light. At these critical moments, NBI demonstrates its outstanding advantages by highlighting abnormal microvascular patterns and mucosal surface structures. This allows physicians to clearly visualize early signs of precancerous or early cancerous lesions, which are potentially curable if identified promptly.
Real-Time Lesion Characterization: Accurate Diagnosis Without Waiting for Biopsy
With NBI, physicians not only see more clearly but can also assess lesion characteristics in real time, reducing dependence on histopathology results. When combined with magnifying endoscopy, this technology allows direct visualization of vascular patterns and microstructures—hallmark indicators used to differentiate benign from malignant lesions.
The introduction of NBI has paved the way for classification systems in early cancer screening, such as JNET, VS Classification, or MESDA-G. These systems enable clinicians to systematically and scientifically categorize lesions, thereby allowing immediate treatment decisions such as EMR or ESD or choosing biopsy if the lesion remains ambiguous—thus shortening the diagnostic and treatment workflow.
Optimizing Endoscopy Workflow: Clear Visualization Without Staining
Another major strength of NBI is its ability to replace traditional chromoendoscopy in many cases. NBI provides high-contrast imaging, allowing clinicians to clearly detect abnormalities without the need for dye agents like indigo carmine or methylene blue. This not only streamlines the endoscopic process but also enhances the experience for both physicians and patients.
Supporting Interventional Endoscopy Like a “Guiding Compass”
For therapeutic procedures such as EMR or ESD, accurately identifying lesion margins and the direction of dissection is critical to success. NBI acts as a “navigational compass,” enabling safer and more precise maneuvers. Pre-procedure, NBI helps define lesion boundaries clearly and select appropriate intervention strategies. During the procedure, it guides the dissection path and highlights submucosal vessels, reducing the risk of bleeding and minimizing complications. Post-procedure, NBI is used to evaluate the margins of resection, ensuring complete removal of diseased tissue (R0 resection) and reducing recurrence rates. In this way, NBI has evolved beyond image enhancement to become a strategic clinical navigation tool.
What’s Special About NBI in the Olympus EVIS X1 System?
Compared to previous generations, the NBI technology in the Olympus EVIS X1 endoscopy system has undergone a comprehensive upgrade in both image quality and clinical effectiveness.
- Improved Brightness: The new NBI light source in EVIS X1 provides bright and clear images even at a distance, addressing the major limitation of older modules. This enables physicians to use NBI from the beginning of the procedure rather than switching modes only when close to a lesion.
- Accurate Image Reproduction: The CV-1500 image processor faithfully reproduces color and enhances contrast between normal and abnormal tissue, making features like blood vessels and mucosal structures sharper and easier to identify, especially when applying classification systems like NICE or JNET.
- Detailed Microstructure Observation: When combined with optical magnifying endoscopy, NBI in the EVIS X1 system allows near-histologic visualization of microvasculature and surface microstructure, helping physicians differentiate between benign and malignant lesions in real time without waiting for biopsy results.
Since its development and integration into Olympus’ modern endoscopy systems, NBI has rapidly become a key tool widely adopted in esophageal, gastric, and colorectal endoscopy. It not only supports early cancer screening but also enhances the quality of diagnosis and therapeutic endoscopy.
As GI cancer screening and treatment efforts intensify, NBI represents not only a technological advancement but also a strategic shift in how physicians approach lesions—seeing more, analyzing deeper, and intervening more precisely. For this reason, NBI is regarded as a powerful “visual weapon” that enhances clinical outcomes and expands the boundaries of modern endoscopy.