[Endostory No.4] Early cancer detection endoscopy: Not a speed race
In cancer screening endoscopy, careful observation and strict adherence to protocols are more important than any high-end technology. There have been many cases where, due to just a few minutes of haste or carelessness, early cancerous lesions were missed, leading to more complex treatment and, in some cases, altering the entire prognosis of the patient.
The clinical case featured in ENDOSTORY #4 is a clear demonstration that with meticulous, systematic observation and the use of image-enhancing techniques, early lesions can be detected and thoroughly managed right in the initial endoscopy.
Case Presentation
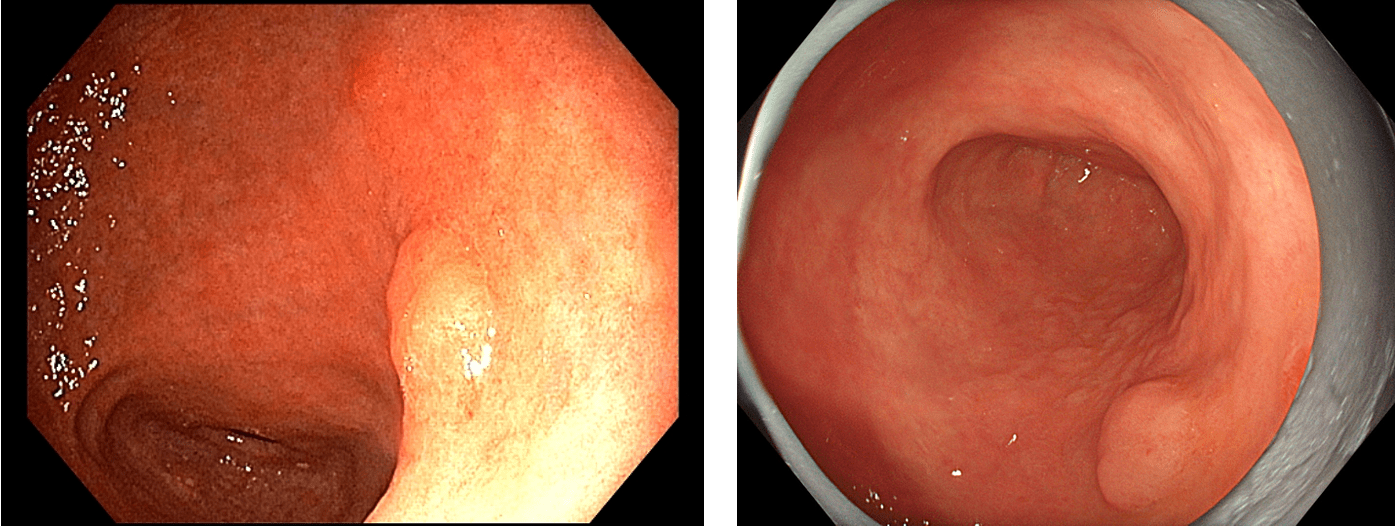
A 62-year-old male patient was admitted for abdominal pain and underwent gastric screening endoscopy. During the examination, the endoscopist identified two simultaneous lesions in the antrum region – a larger lesion along the lesser curvature and a smaller one on the posterior wall of the antrum. This is a typical case of multifocal gastric cancer, which is not uncommon but easily missed if the endoscopic procedure is not performed carefully and systematically.
How to ensure all lesions are detected?
In practice, many young doctors, especially those new to early cancer screening, tend to focus too much on the first lesion they find, inadvertently overlooking the rest of the gastric mucosa. Studies from Japan and South Korea show that multifocal gastric cancer accounts for 4–10% of early gastric cancer cases, which means that stopping the examination after detecting just one lesion risks missing a second one.
To minimize this risk, in this case, the physician performed a sequential, thorough observation and analysis to accurately identify and evaluate all lesions and ensure no suspicious areas were overlooked.
Observation and Lesion Evaluation Procedure
Note: The following sequence reflects the approach taken by the physician in this particular case. In real-world practice, each doctor may arrange observation techniques based on experience, available equipment, and lesion characteristics. This article provides a reference example of a detailed, systematic analytic flow, not a universal protocol.
Initial Observation with White Light Imaging (WLI)
A full inspection of the gastric mucosa using white light imaging (WLI) helps identify natural morphology and detect suspicious abnormalities. In the initial images, the lesion on the lesser curvature of the antrum appeared as a flat, elevated area of about 30 mm on a background of atrophic mucosa with intestinal metaplasia.
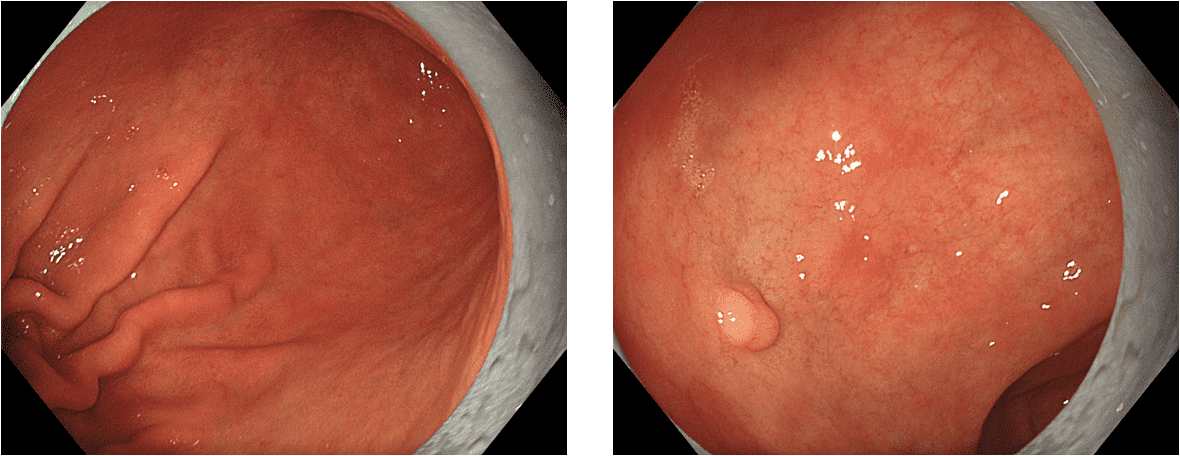
Note: Over-insufflation during WLI observation can stretch the mucosa, making flat 0-IIa lesions harder to identify. Adjusting the level of air insufflation flexibly is crucial to avoid missing flat lesions.
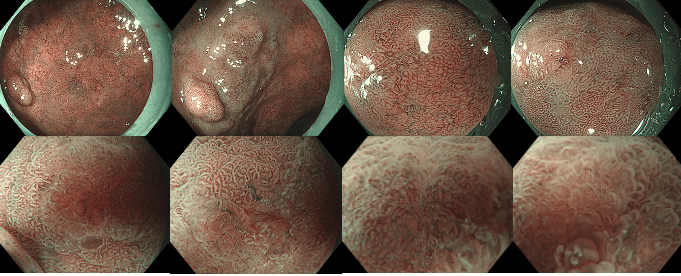
Enhancing Image Contrast with TXI
After identifying the suspicious area using WLI, the physician switched to TXI (Texture and Color Enhancement Imaging) to enhance contrast and highlight the lesion. TXI clarified the boundary and color difference between the lesion and surrounding mucosa—an essential step before applying dye.
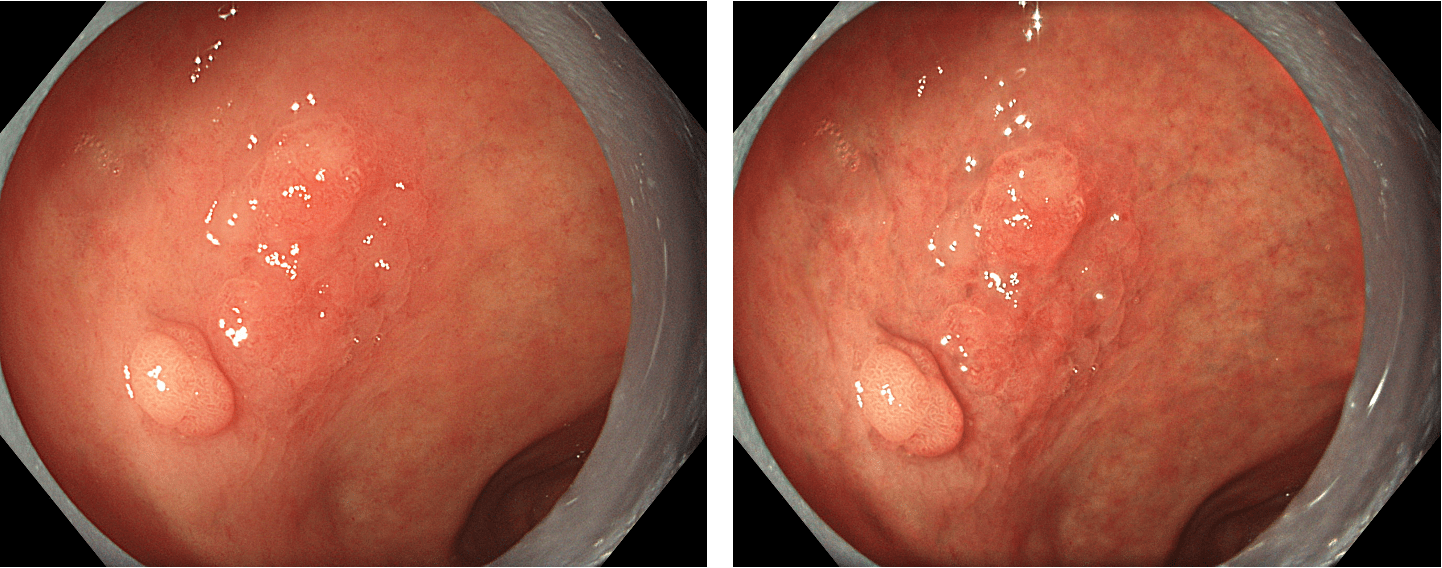
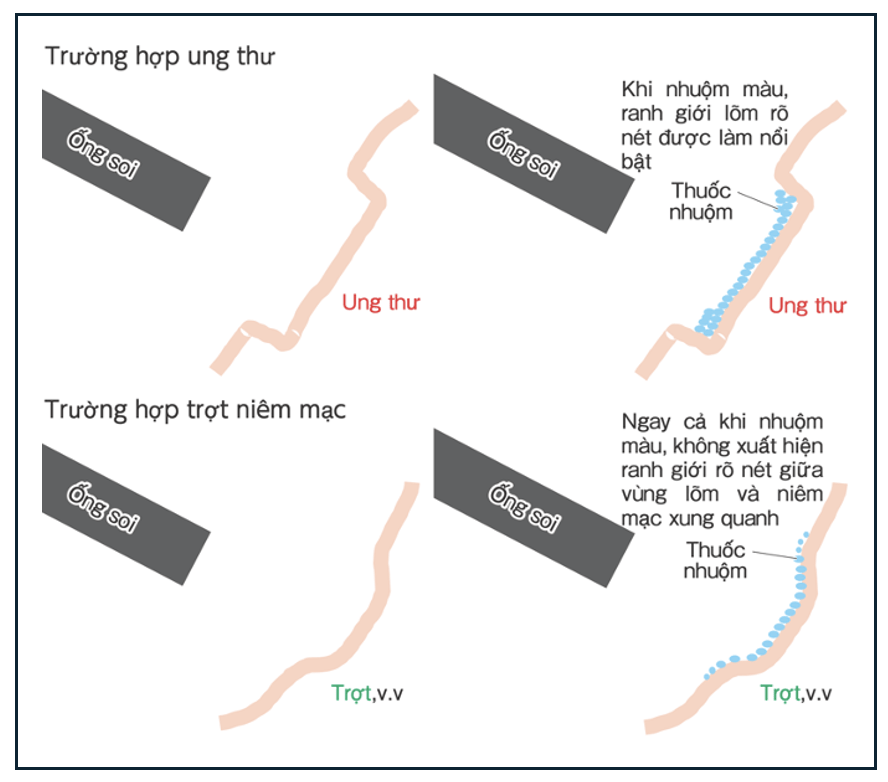
Indigo Carmine – A Powerful Tool to Uncover Subtle Lesions
Once a suspicious area was identified with WLI and TXI, Indigo Carmine dye was sprayed over the mucosal surface. This dye does not absorb into cells but spreads and pools in grooves, depressions, or irregular structures, making flat lesions more distinguishable from healthy mucosa.
Observation time post-spray is typically short (30–60 seconds). This method is especially effective in cases with background mucosa showing atrophy or intestinal metaplasia, which can obscure lesion boundaries. Currently, at K Hospital, a 0.4% Indigo Carmine solution is commonly used in early gastric cancer screening.
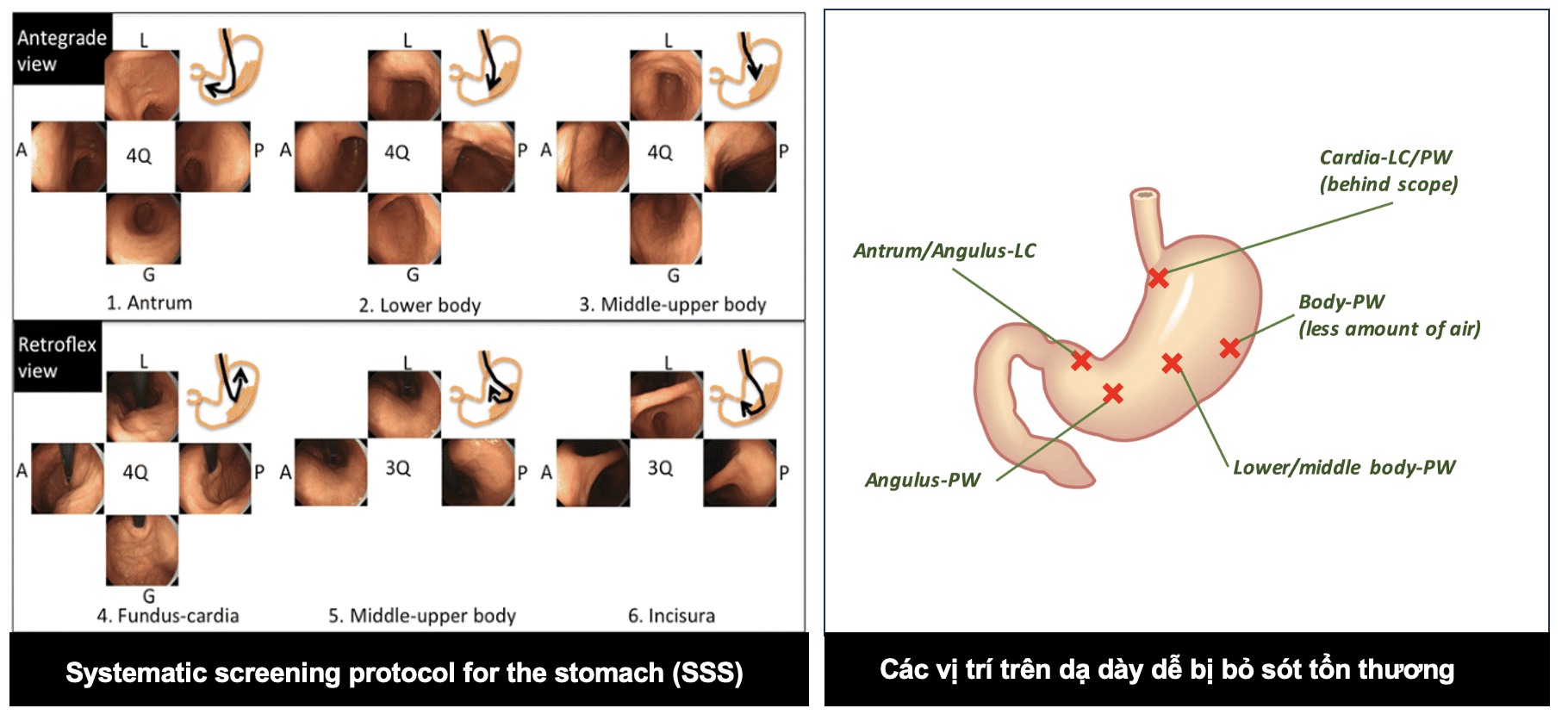
Applying SSS – Systematic Screening of the Stomach to Avoid Oversight
Even when a lesion is clearly seen, the SSS (Systematic Screening of the Stomach) protocol of taking 22 standardized images should be followed. This ensures that the entire gastric mucosa is screened, especially high-risk areas such as the posterior antrum – precisely where the second lesion in this case was detected.
To perform SSS, in the forward view, endoscopic images are taken of the four quadrants of the antrum, and the lower, middle, and upper parts of the gastric body. Then, in the retroflexed view, four quadrants of the fundus and cardia are captured. Next, three additional quadrants of the middle and upper gastric body and the lesser curvature are imaged. This results in a total of 22 gastric endoscopic images.
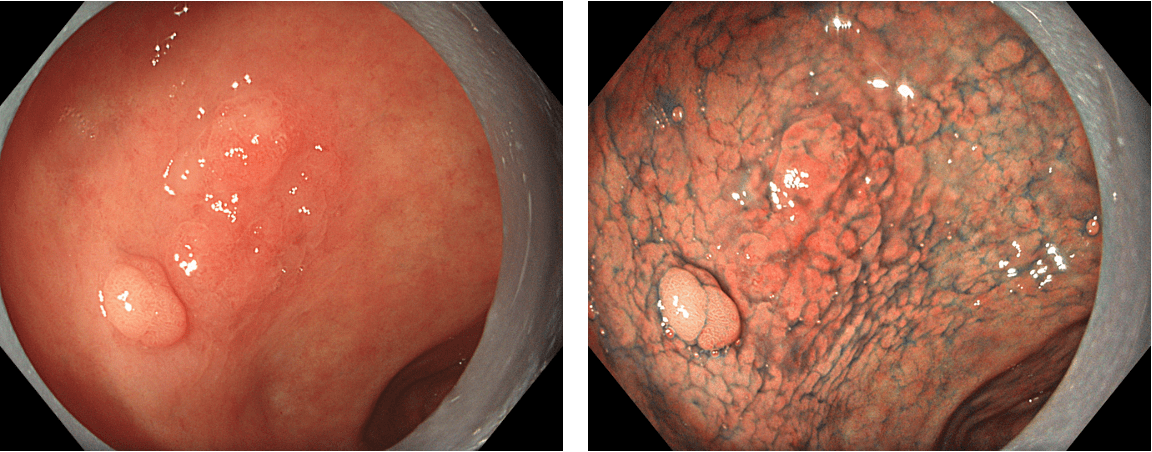
Detailed Microvascular Analysis with Magnified NBI
Finally, NBI (Narrow Band Imaging) and magnified NBI were used to evaluate the microsurface (IMSP) and microvascular (IMVP) patterns of the lesion. The magnified image revealed a clear demarcation line, abnormal microvascular structure, and heterogeneous WOS (white opaque substance) distribution—features suggestive of differentiated adenocarcinoma. This informed the decision for ESD and risk stratification.
Intervention and Pathology Results
Both lesions were completely resected via Endoscopic Submucosal Dissection (ESD) in a single session.
- First lesion pathology: Moderately differentiated adenocarcinoma (pT1a), confined to the mucosa, no lymphovascular invasion, negative resection margins.
- Second lesion pathology: High-grade dysplasia (HGD).
This is considered curative treatment with a good prognosis if follow-up is conducted on schedule.
So, how long should an endoscopy take?
Observation time is a key factor in detecting early gastric cancer. Is there a recommended minimum time to ensure thorough examination? The answer is yes.
- Teh JL et al. (2020, Gut): Physicians who observed the stomach for ≥7 minutes (excluding biopsy time) had significantly higher detection rates compared to those who observed for <3 minutes.
- ESGE Guidelines: Recommend ≥7 minutes for adequate mucosal inspection.
- JGES (Japan Gastroenterological Endoscopy Society): Suggest a minimum of 3–5 minutes, with encouragement for more detailed observation.
In summary, the optimal observation time for gastric endoscopy should be at least 3 minutes, especially for early cancer screening or suspicious cases (not including insertion, biopsy, or therapeutic time). Recommended practices include:
- Capturing a minimum of 8–10 standard images (cardia, fundus, greater/lesser curvatures, antrum, angle, pylorus), ideally up to 22 via Prof. Yao’s SSS protocol (*), or even 40 images as practiced in Japan (**).
- Cleaning mucosa and using simethicone for defoaming.
- Applying magnification or chromoendoscopy if lesions are suspected.
Conclusion
Early cancer screening is never a race against time. It is a journey of patience, discipline, adherence to protocols, and the ability to flexibly integrate various imaging techniques. A moment of more careful observation or a slightly more cautious angle can make all the difference between early and late, between loss and preservation. At that point, endoscopy becomes not just a technical skill, but a reflection of dedication and deep respect for life.
(*) Prof. Yao: Professor Katsunori Yao, who proposed the Systematic Screening of the Stomach (SSS) method.
(**) 40-image protocol: A rigorous standard currently practiced at several leading endoscopy centers in Japan (and some in South Korea).
About ENDOSTORY
ENDOSTORY is a clinical endoscopy storytelling series presented by Lenus Vietnam, with the aim of providing practical and valuable insights for endoscopists. Every Friday at 8:00 PM, a selected clinical “story” is posted on Lenus Vietnam’s fanpage.
The series is professionally advised by Dr. Tran Duc Canh, an expert in early cancer diagnosis and treatment. As a seasoned ESD practitioner and a mentor to many young endoscopists in Vietnam, Dr. Canh’s commitment to sharing and spreading knowledge is a major inspiration behind the birth of the ENDOSTORY journey.
As the series is still in its early stages, we welcome any feedback or suggestions. Please message the Lenus Vietnam fanpage or email us at [email protected] so we can hear your voice.