[Endostory #5] Effective and safe endoscopic intervention starts with a correct understanding of the electrosurgical unit (ESU)
In most modern interventional endoscopic procedures such as EMR, ESD, or polypectomy, one device plays a crucial role in determining the effectiveness of cutting, coagulation, and the overall safety of the procedure: the Electrosurgical Unit (ESU).
In reality, for many young endoscopists, the ESU remains a “black box,” with various modes like Endo Cut, Forced Coag, or Swift Coag often used based on habit or simply because “that’s how the teachers do it.” A clear understanding of the ESU’s principles not only builds confidence during procedures but can often be the deciding factor between a successful intervention and an undesirable complication.
What is the ESU?
The ESU (Electrosurgical Unit) is a device that generates high-frequency alternating current (>100,000 Hz) and transmits this current through instruments such as electrosurgical knives, snares, or forceps to generate heat on the tissue. The high frequency avoids unwanted neuromuscular responses and focuses the energy on biological tissue effects—namely cutting and coagulation.
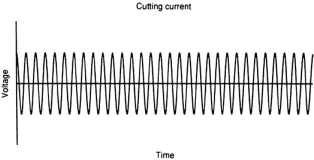
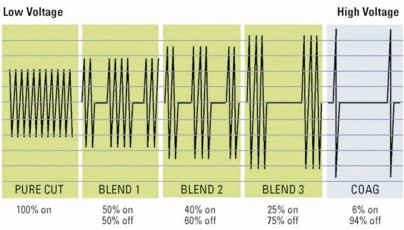
There are three main types of electrical currents generated by the ESU: cutting (Cut), coagulation (Coag), and blended (Blend).
Cut Mode
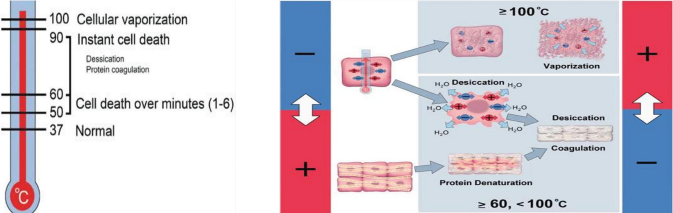
Cut mode uses continuous AC current with voltage ≥200V, rapidly raising tissue temperature to cause intracellular water to evaporate and rupture cell membranes, producing a sharp cutting effect. Because the heat is concentrated, coagulation is minimal, enabling precise incisions with limited collateral damage.
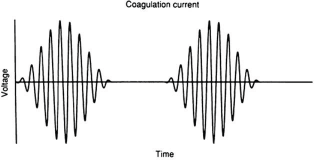
Coagulation Mode
Coag mode uses interrupted current at high voltage (usually around 1,000 Vp), producing slower heating that dehydrates tissue and denatures proteins, achieving coagulation without cellular rupture. The strength of coagulation depends on voltage and pulse cycle.
Blend Mode
Blend mode combines cutting and coagulation by adjusting the duty cycle (on/off timing of the current). The longer the “on” phase, the stronger the cutting; the shorter, the more dominant the coagulation. This mode allows simultaneous cutting and hemostasis, ideal for interventions requiring flexible control.
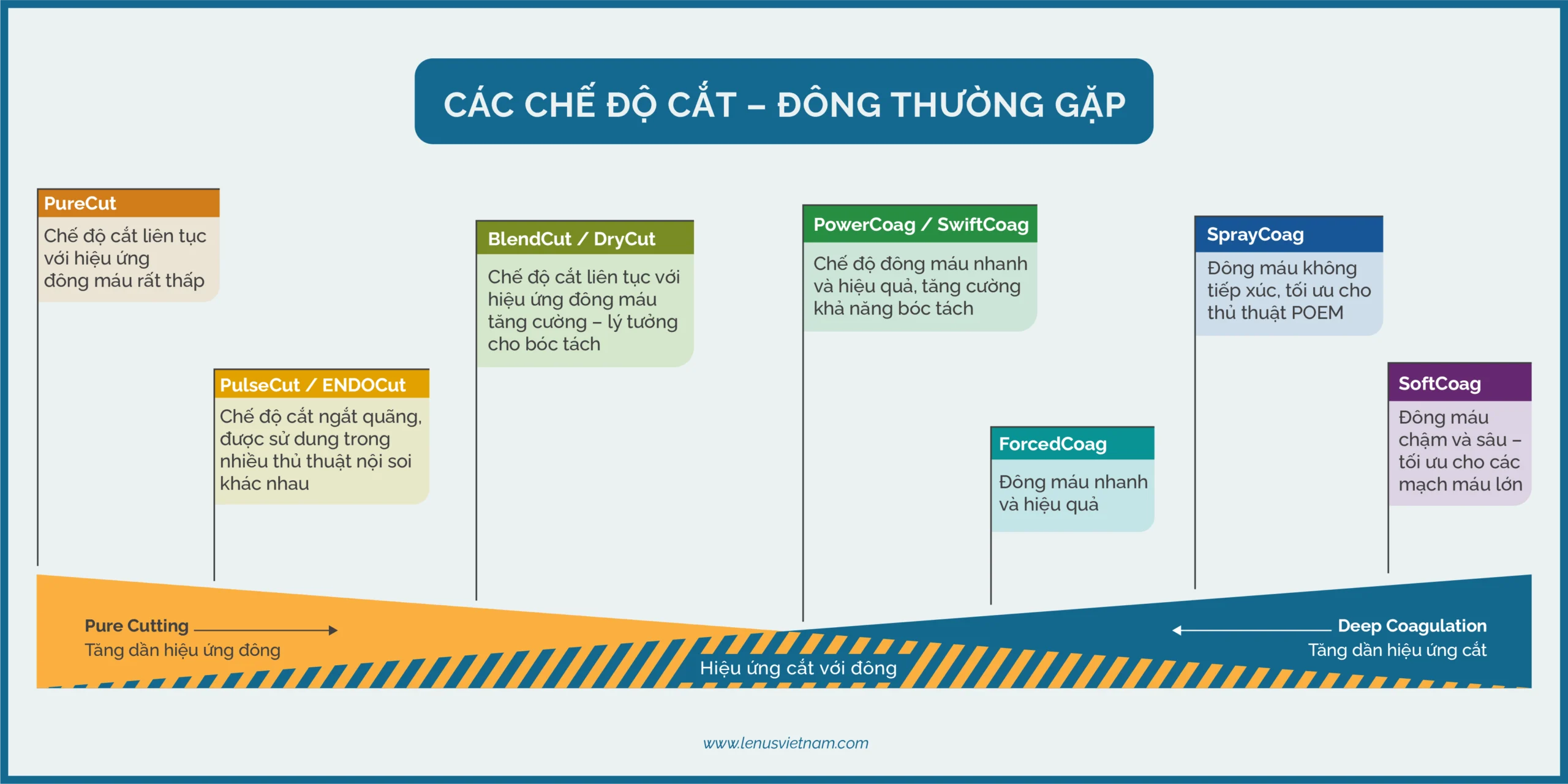
Common Cutting and Coagulation Modes in Interventional Endoscopy
Modern ESU systems have made significant advances by integrating intelligent software that enables fine and precise control of electrical currents. Physicians can now choose from various output modes to optimize cutting and coagulation effects based on specific clinical contexts. Below are common ESU modes and their uses in interventional endoscopy:
Endo Cut (similar to Olympus’ Pulse Cut)
This is a widely used blended mode. Current is delivered in cycles: a short cutting phase (DURATION) alternates with a coagulation phase. The operator can adjust EFFECT (degree of coagulation) and INTERVAL (time between cycles), allowing precise cut–coag rhythms. Often used for mucosal or fibrotic tissue incision.
- EFFECT 1: No coagulation
- EFFECT 2: Soft Coag
- EFFECT 3, 4: Forced Coag
Endo Cut I and Q differ by voltage control depending on instrument type (I for metallic instruments, Q for snare).
Note: Endo Cut is primarily a cutting mode with minimal coagulation. Commonly used for mucosal incision and submucosal dissection.
Dry Cut (similar to Olympus’ BlendCut mode)
Dry Cut is a cutting mode with enhanced coagulation, using 600–800 Vp at EFFECT 2–4. It is used when precise submucosal dissection is needed, or for mucosal incision in highly vascularized areas.
Note: Due to increased heat, Dry Cut should be used carefully to reduce deep thermal damage, minimize contact time, and ensure wide incision margins for better histopathological evaluation.
Swift Coag (similar to Olympus’ PowerCoag mode)
Swift Coag is a coagulation mode with mild cutting capability, operating at 850–1,050 Vp (EFFECT 2–4). It provides stronger coagulation than Dry Cut but less than Forced Coag; cutting ability is less than Dry Cut but more than Forced Coag.
Thanks to its combined mild cut and coagulation effects, Swift Coag is often preferred over Forced Coag for precise hemostasis of blood vessels during mucosal dissection. It is favored for submucosal dissection with specific knives.
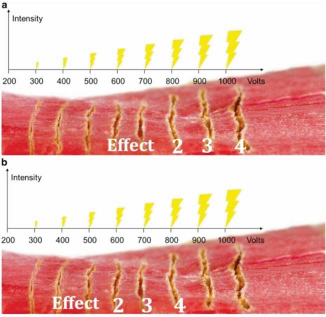
Forced Coag
One of the most powerful coagulation modes. It uses intermittent current at high voltage (~1000V), creating deep thermal injury to “seal” vessels quickly—especially useful in vascular-rich areas. However, careless use can lead to carbonization and compromise histological evaluation. It should be used with proper instrument motion to avoid carbonization.
With Forced Coag, the EFFECT setting controls the coagulation effect. The higher the EFFECT, the greater the voltage, resulting in deeper and wider tissue damage, thereby enhancing hemostatic efficacy. However, a high EFFECT also increases the risk of tissue charring and carbonization, which may interfere with pathological evaluation.
Soft Coag
A pure coagulation mode using low voltage (<200V), creating coagulation without cutting or carbonization. Often used for proactive hemostasis with hemostatic forceps or for marking tissue with an electrosurgical knife.
In Soft Coag, low EFFECT means slower increase in tissue impedance and current power dropping closer to zero, resulting in deeper and stronger tissue effects at low settings.
Spray Coag
A “non-contact” coagulation mode using very high continuous voltage (up to 4,000 Vp) and a low duty cycle (~6%), producing electrical discharge onto adjacent tissues.
Thanks to wide-area hemostasis, Spray Coag is preferred in POEM or submucosal tunneling procedures where contactless dissection is needed.
Tissue Effects Depend on More Than Just the ESU Mode
Cutting or coagulation efficiency is not determined solely by ESU settings. It also depends on various biological and technical factors. According to Ohm’s Law, voltage and tissue impedance determine current intensity—key to electrosurgical effects.
- Tissue resistance varies by type: fatty or fibrotic tissue (often seen post-biopsy or in submucosal fibrosis) has higher resistance, favoring coagulation and making cutting harder without increased voltage.
- Current intensity depends on contact area: smaller knife → higher current density → better cutting; larger surface area → dispersed current → weaker cut and broader thermal injury.
- Amount of tissue in contact affects cutting: more tissue → lower cutting efficiency, higher risk of carbonization.
- Speed and movement: Fast movement may gather more tissue, lowering current intensity and cutting effect while increasing deep thermal injury. Slow, steady movement with short duty cycle gives more controlled burning but may risk carbonization. Therefore, controlling speed and pressure direction is crucial.
Understanding these principles is particularly helpful in ESD, allowing physicians to adjust current intensity for desired effects (e.g., cutting fibrotic tissue without carbonization, coagulating vessels before cutting, cutting with hemostatic forceps without burning) by changing device, target tissue amount, or movement speed.
Clinical Applications
[Reference] Common settings for ESD interventions used in specialized ESD centers worldwide (based on ERBE ESU VIO300D model)
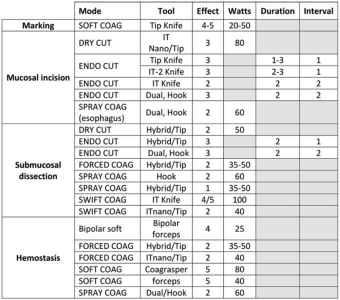
Specific electrosurgical modes corresponding to ESD procedural steps:
- Mucosal incision: This is commonly performed using the ENDO Cut mode. Some prefer Dry Cut or Swift Coag depending on the knife type and anatomical location.
- Submucosal dissection: Forced Coag is used with appropriate knife movements (manual manipulation) to avoid carbonization. In fact, Swift Coag or Dry Cut are increasingly popular due to their better cutting ability, especially in areas with fewer blood vessels. These modes are not limited to specific regions and can be flexibly switched depending on the nature of the vessels and tissues to achieve optimal dissection.
- Hemostasis: If the vessel diameter is less than 1 mm, Forced Coag, Dry Coag, or Swift Coag are all effective. For larger vessels, active coagulation with hemostatic forceps using Soft Coag is strongly recommended. Soft Coag mode is effective even in underwater conditions.
In special situations:
- Fibrosis: In fibrotic tissue with low water content, carbonization is more likely when using coagulation currents. Therefore, cutting modes like Endo Cut are preferred, with careful dissection of small areas. In cases of less dense fibrosis, Dry Cut is also a suitable option.
- Highly vascular structures: In vascular-rich tissue, often seen in cancerous lesions, coagulation efficiency should be increased to avoid bleeding during dissection. Forced Coag is effective but easily causes carbonization. When simultaneous cutting and minimized thermal injury are needed, Swift Coag or Dry Cut are more optimal. If bleeding persists, it is recommended to increase the EFFECT or power (Watts), actively coagulate with forceps using Soft Coag, and then continue dissection using Endo Cut.
- POEM procedure: In POEM, since the submucosal layer is poorly vascularized, dissection is usually easy. Muscle cutting using Spray Coag helps reduce bleeding due to its widespread coagulation effect, but care should be taken to separate the circular muscle from the longitudinal muscle before cutting to avoid deep injury. Endo Cut with a high EFFECT can also be used as an alternative in certain cases
How are the ESU cutting-coagulation modes applied in a typical ESD case?
Let’s take a look at a typical ESD procedure at K Hospital for a comprehensive view of how the doctors there strictly apply the Japanese endoscopic intervention protocol, as well as “master” the ESU to ensure safe and effective procedures for the patient.
Pre-intervention preparation:
- Personnel preparation:
– General practitioner with gastrointestinal endoscopy certification, trained in early GI cancer diagnosis and intervention. - Equipment and tools:
– Equipment: Olympus CV 190 endoscopy system; Electrosurgical units: ERBE, Olympus; Irrigation system
– Tools: dissection knives, injection needles, hemostatic forceps, overtip, submucosal lifting solution, indigo carmine dye - Patient preparation:
– Medical examination and review of patient records
– Explanation provided to patient and family
– Signing of consent forms - Anesthesia for the patient:
– Drugs: Pethidine 35 mg i.v, Midazolam 2–4 mg i.v, Propofol 10 mg/ml
– Attention to patients with underlying conditions
– Continuous monitoring using a monitor
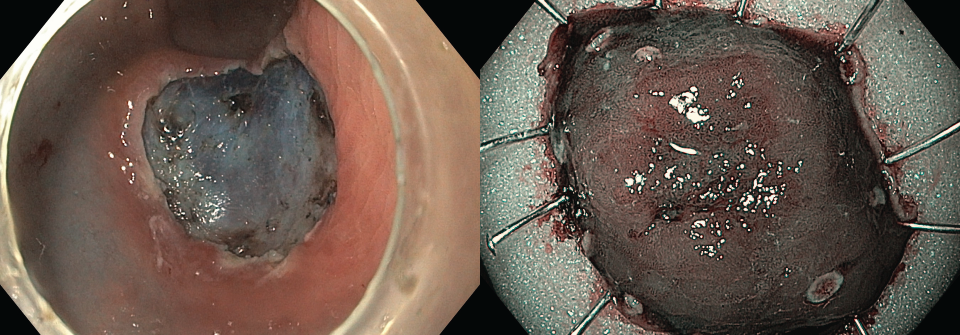
Clinical procedure of ESD in a real case:
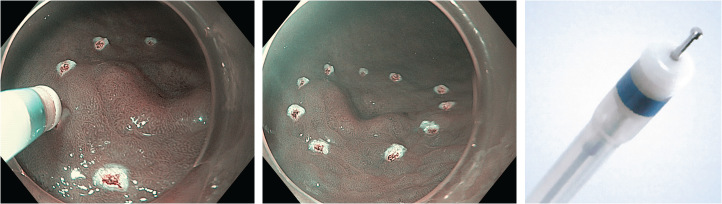
Step 1: Lesion marking / Marking
- Mode: Soft Coag
- Reason for choosing Soft Coag: low voltage (<200V), does not cause cutting or tissue burning, very safe for marking around the lesion using a knife.
- Tool: Olympus Dual Knife
Step 2: Injection and mucosal entry hole / Injection – Marking hole
- Mode: Endo Cut I – EFFECT 2
- Tool: Olympus DualKnife
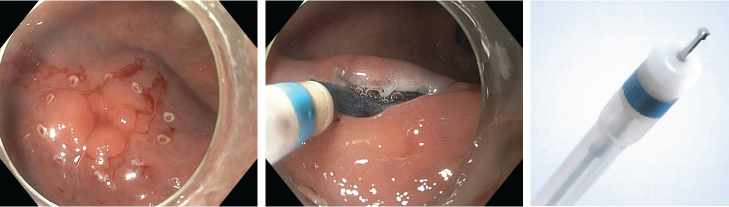
Step 3: Circumferential cutting / Circular cutting – Deeper cutting
- Mode: Endo Cut I – EFFECT 2
- Tool: Olympus ITknife2
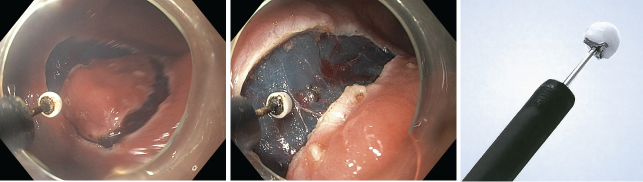
Step 4: Submucosal dissection
- Mode: Forced Coag – Mode 6.5
- Tool: Olympus ITknife2
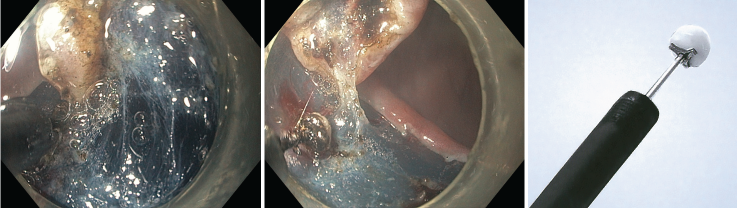
Total procedure time: 30 minutes
Histopathology result: In situ well-differentiated adenocarcinoma, no vascular or lymphatic invasion (tub1, pTis, Ly0, V0)
Conclusion
Through each step of a real ESD case, it is clear that the ESU is not merely a power source for cutting and coagulation, but rather a vital energy control tool that proves most effective when the physician clearly understands each mode and selects the right time for use.
In a complex field such as medicine in general and therapeutic endoscopy in particular, it is difficult to define a single “standard” mode or approach for all cases. The only real “standard” is the constant learning, deep understanding, and critical thinking of medical professionals to proactively ensure safety, precision, and reliability for patients.