[ENDOSTORY #6] Small but not negligible lesion: EMR or ESD – which is the safe choice?
A female patient came to the hospital due to epigastric pain, a fairly common symptom in clinical practice. The patient had a healthy medical history, subclinical examinations including CT scan showed no abnormalities, abdominal ultrasound was normal, complete blood count and biochemistry tests were all normal.
A small lesion revealed
White light endoscopy recorded a small depressed lesion (0-IIc) at the antrum, greater curvature, slightly reddish in color, about 10mm in size. The lesion was non-ulcerated, the mucosal surface was regular, not firm, not raised, with no signs suggesting submucosal invasion.
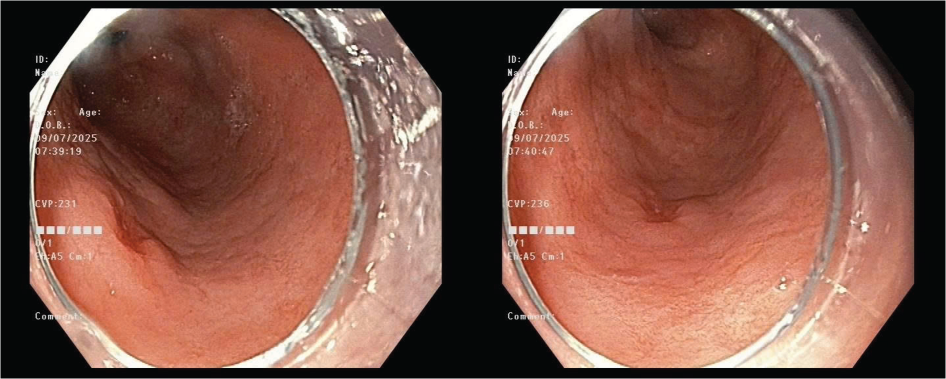
However, when switching to NBI with magnification, the situation changed completely with signs according to the VS classification suggesting this could be a non-benign lesion:
- Clearly defined lesion boundary
- Abnormal microvascular architecture
- Abnormal surface pattern
Based on M-NBI endoscopic imaging, the physician diagnosed the lesion as well-differentiated T1a cancer.
EMR or ESD – should intervention decisions rely only on size?
For T1a, non-ulcerated (UL0), well-differentiated lesions and ≤2cm in size, according to the Japanese Gastric Cancer Treatment Guideline 2021, endoscopic indication is absolute.
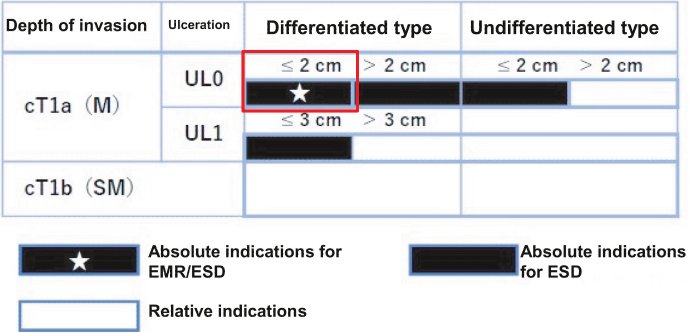
However, the choice between EMR or ESD remains a common question, especially when the lesion appears “easy to manage.”
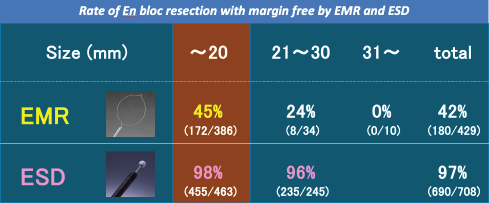
EMR has the advantage of being quick and cost-saving for the patient, but the en bloc resection rate is very low. According to studies in Japan, even for lesions <2cm, the en bloc resection rate with EMR is no more than 50%. Meanwhile, in terms of en bloc resection efficacy, ESD shows a superior rate up to 98%. Therefore, in this case, although the lesion belongs to the ≤2cm, non-ulcerated group — usually the overlapping zone between EMR and ESD — but with the goal of achieving R0 resection (complete lesion removal), avoiding piecemeal resection, and the need for complete margin evaluation, ESD was chosen.
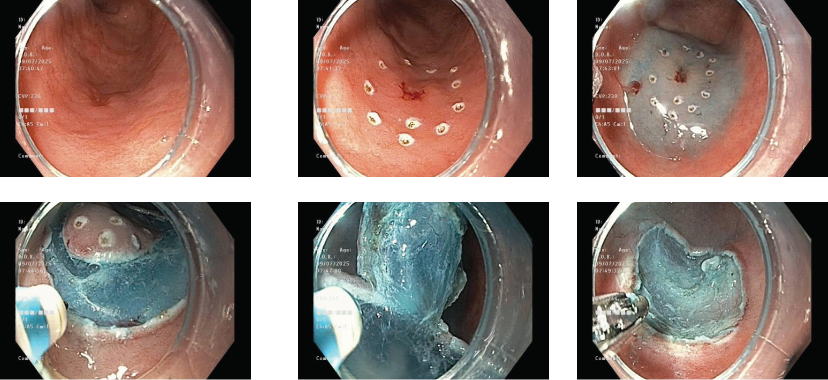
The ESD procedure proceeded smoothly within 15 minutes:
- Lesion marking: Olympus Dual Knife
- Submucosal injection: Non-lifting sign (-)
- Circumferential cutting: Olympus Dual Knife, IT Knife, ESU EndoCut EFFECT 2 mode
- Submucosal dissection: Olympus Dual Knife, IT Knife 2, EndoCut EFFECT 2 & ForceCoag 65W mode
- Hemostasis: SoftCoag 60W
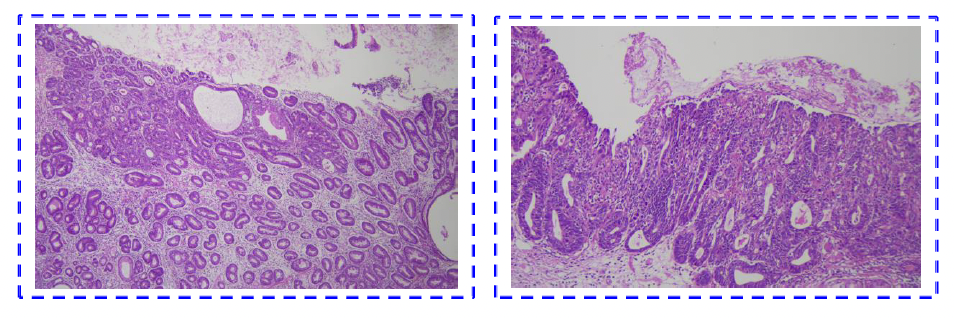
eCura – A system to evaluate curability after ESD
After completing ESD, the question is not only “has it been completely removed,” but also “is it safe enough for follow-up, or will additional surgery be needed?”
To answer that, the eCura system was developed to help doctors assess the curability level of ESD in early gastric cancer treatment, based on histopathological data collected after ESD. With eCura – evaluation factors include:
- Histological type: differentiated (diff-type) or undifferentiated (undiff-type)
- Depth of invasion: T1a or T1b
- Ulceration status: UL
- R0 resection margin clearance
- Lymphovascular invasion (Ly, V)
- Margin safety distance (HM, VM)
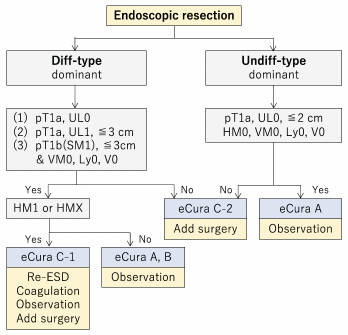
Accordingly, post-ESD lesions will be classified into groups:
- eCura A: Completely curative → only needs regular follow-up
- eCura B: Low risk → can be followed up or consider additional treatment
- eCura C-1/C-2: High risk → need to consider radical surgery
The eCura system helps physicians make decisions after ESD, limiting unnecessary surgeries and improving long-term follow-up outcomes for patients.
In this clinical case, based on eCura, the lesion was evaluated as eCura A, with the next management direction being regular follow-up.
Conclusion
This clinical case emphasizes an important point: small lesion does not mean simple. Accurate assessment without subjectivity – choosing the right technique – complete curative management from the beginning is the foundation to optimize prognosis and reduce long-term burden for the patient.
Reference:
Japanese Gastric Cancer Treatment Guideline 2021 (6th edition)
About ENDOSTORY
ENDOSTORY is a series sharing real-life gastrointestinal endoscopy cases conducted by Lenus Vietnam, aiming to bring useful information to endoscopists. Every week, one “story” will be selected and posted on Lenus Vietnam’s fanpage at 8:00 PM every Friday.
The series is medically advised by Dr. Tran Duc Canh – an expert in early cancer diagnosis and treatment. Not only has he participated directly in many complex ESD cases, Dr. Tran Duc Canh is also a teacher who has trained many young Vietnamese endoscopists in ESD techniques, contributing to the widespread adoption of this technique considered the “golden key” in early gastrointestinal cancer treatment. His spirit of sharing to spread knowledge is one of the inspirations for the creation of this ENDOSTORY journey.
The program is taking its first steps and greatly needs feedback for improvement. All feedback/discussion please inbox Lenus Vietnam fanpage or send to email [email protected] so we can hear from you.