[ENDOSTORY #7] TYPE R Vascular pattern: A warning sign of malignancy not to be missed
An 82-year-old male patient was admitted to the hospital after an abnormal esophageal lesion was detected during endoscopy at a local medical facility. The lesion appeared as a firm elevated mass, approximately 12mm in size, with suspicion of malignancy. The patient had a history of hypertension. Initial paraclinical investigations showed: blood tests within normal limits, abdominal ultrasound revealing gallbladder stones, chest X-ray and CT showing no abnormalities; abdominal CT additionally noted a mesenteric cyst.
Let’s follow ENDOSTORY #7 as we explore the process of evaluating and determining the invasion depth of the lesion and learn about the appearance of a critical warning sign of malignancy that must not be overlooked.
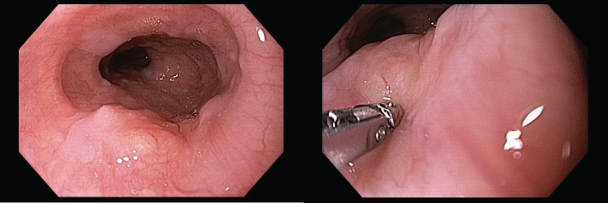
White-light imaging: A firm, immobile elevated lesion
White-light endoscopy revealed an elevated lesion in the middle third of the esophagus, approximately 30cm from the upper dental arch. The surface appeared uneven but relatively smooth, with disrupted mucosal continuity. Biopsy probe examination indicated a firm, immobile lesion, suggestive of submucosal or invasive pathology.
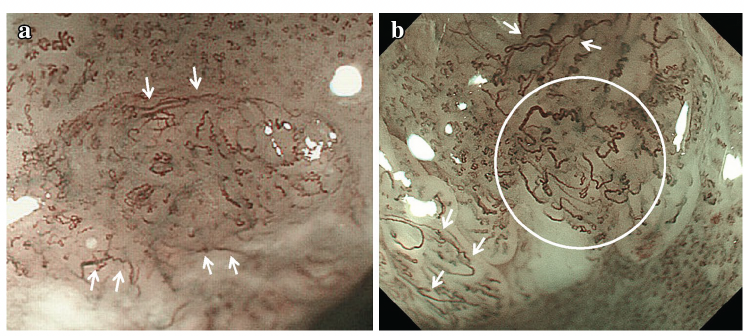
NBI abnormalities and the role of Type R microvascular pattern
Low-magnification NBI imaging showed a brown color negative (BC−) area, similar to typical squamous cell carcinoma (SCC) lesions, due to increased subepithelial microvascular density.
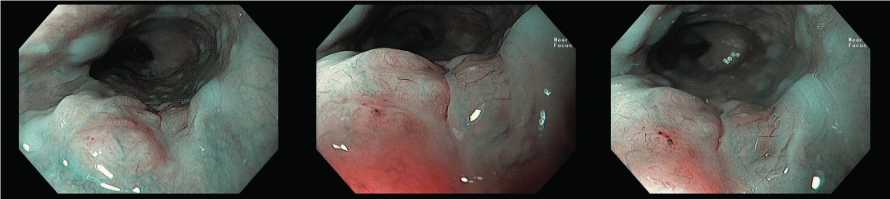
On high-magnification NBI, the vascular structures in the suspicious area appeared dilated, thin, tree-like branched, lacking loops, disorganized, and without clear borders from adjacent normal mucosa features characteristic of the Type R (Reticular) vascular pattern.
Type R vessels represent an abnormal microvascular morphology often seen in poorly differentiated invasive SCC or rare cancer types such as adenosquamous carcinoma and neuroendocrine carcinoma. These vessels form due to loss of cellular adhesion, allowing cancer cells to spread diffusely without forming structured nests, which results in a characteristic reticular capillary network. Identifying Type R patterns enables clinicians to suspect undifferentiated/invasive cancers early—types that are difficult to detect using conventional morphological criteria.
It is important to note that in some cases, chronic inflammatory lesions may also present with non-looped vessels, termed Type B2i. To distinguish these from Type R, note that Type B2i vessels have a very dense and uniform diameter, without the reticular branching seen in Type R.
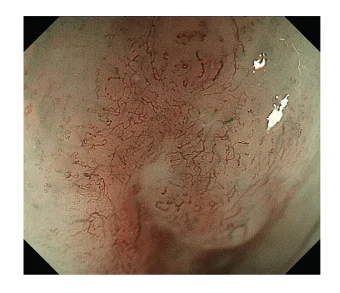
EUS and its role in evaluating the depth of invasion
After identifying suspicious features with magnified NBI—especially the presence of Type R vessels suggesting poorly differentiated, deeply invasive carcinoma—the physician indicated endoscopic ultrasound (EUS) to assess the lesion’s depth of invasion into the esophageal wall, in conjunction with CT and PET-CT for staging.
EUS revealed a hypoechoic lesion disrupting the continuity of the submucosal layer but not yet invading the muscularis propria. This is a crucial factor for staging and treatment planning, as submucosal-invasive cancers are typically no longer eligible for endoscopic submucosal dissection (ESD) alone and may require surgery or chemoradiotherapy.
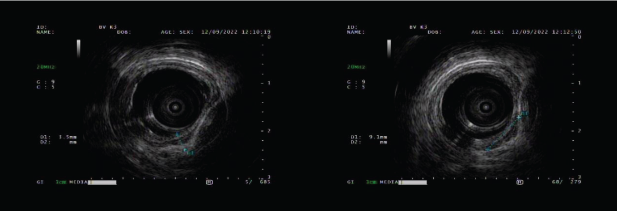
In this case, EUS not only confirmed suspicions raised by NBI imaging but also helped avoid missing deeply invasive lesions—particularly poorly differentiated types with unclear boundaries on white-light and standard NBI imaging. Combining information from both techniques enhances diagnostic accuracy in cancer staging and helps personalize treatment strategies for each patient.
Conclusion – Key Takeaways
Type R vascular pattern—though not yet widely recognized in routine endoscopic practice—holds significant practical value in helping endoscopists detect poorly differentiated cancer types early, which often elude conventional endoscopic detection.
Continuous updates on new medical knowledge, along with flexible integration of various endoscopic technologies (NBI, EUS…), are key to enhancing diagnostic capabilities for clinicians.
About ENDOSTORY
ENDOSTORY is a clinical case series in gastrointestinal endoscopy presented by Lenus Vietnam, aiming to provide practical and useful information for endoscopists. Each week, one selected “story” is posted on the Lenus Vietnam fanpage at 8:00 PM every Friday.
This series is professionally advised by Dr. Tran Duc Canh—a specialist in early cancer diagnosis and treatment. Not only has he been directly involved in numerous complex ESD cases, but he also trains many young endoscopists in Vietnam in this advanced technique—considered the “golden key” in early GI cancer treatment. His spirit of sharing and spreading knowledge is a core inspiration behind the ENDOSTORY journey.
As the series is still in its early stages, we welcome all feedback to improve. Please inbox Lenus Vietnam fanpage or email us at [email protected] to share your thoughts.