ENDOSTORY #13: FROM JES CLASSIFICATION TO THE DECISION OF ESD IN AN EARLY ESOPHAGEAL CANCER CASE
Early esophageal squamous cell carcinoma is often recognized through very subtle and “delicate” changes. Sometimes, just a small area of abnormal blood vessels can completely alter the treatment strategy. In this ENDOSTORY #13, we follow a case where the JES classification played an important role in helping the doctor decide whether to perform ESD or not.
We present the case of a 75-year-old male patient, with no medical history, who came for a routine health check-up and was found to have an esophageal lesion.
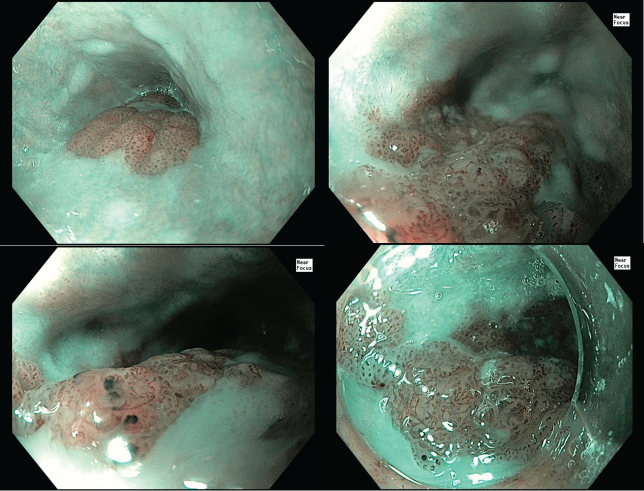
Initial observation with WLI
With white light imaging, a lesion was observed involving one-third of the esophageal circumference, located in the upper third, 23–26 cm from the incisors. Its gross morphology was slightly elevated, classified as Paris type 0-IIa. The lesion appeared redder than the surrounding mucosa, and its distensibility was relatively good.

Observation with NBI
Under NBI, a clearly demarcated brownish area, BC(+), was seen—darker than the surrounding normal mucosa, a common sign of esophageal squamous cell carcinoma.
According to the JES classification, the doctor noted type B1 vascular pattern (abnormal loop-like vessels with all four features: dilation, tortuosity, irregular caliber, and irregular shape → suggesting superficial invasion EP/LPM) and a small area of type B2 vessels (abnormal, fewer loop formations → suggesting shallow invasion MM/SM1).
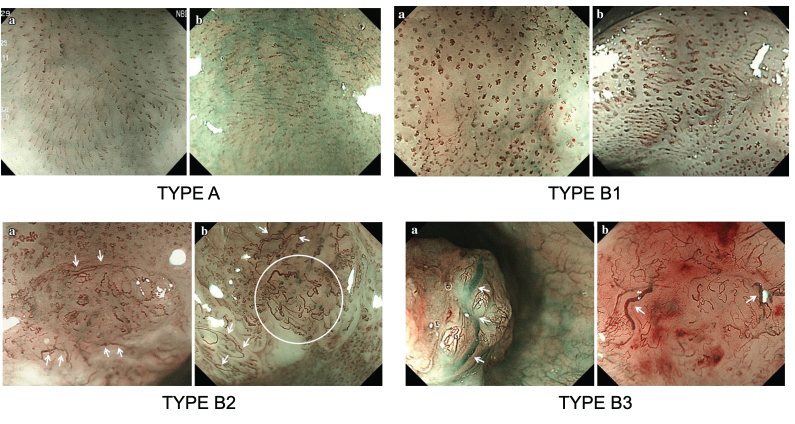
Prediction of SSCC invasion depth based on vascular patterns according to JES classification
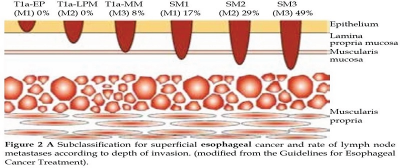
First, let’s review the terminology for invasion depth according to JES classification:
- SIN (squamous intraepithelial neoplasia): precancerous squamous intraepithelial lesion
- EP (Epithelium): intraepithelial squamous cell carcinoma, confined to the epithelium, no lymph node metastasis risk
- LPM (Lamina Propria Mucosae): carcinoma invading lamina propria, very low risk of nodal metastasis, typical indication for ESD
- MM (Muscularis Mucosae): carcinoma invading muscularis mucosae, higher nodal metastasis risk than LPM
- SM (Submucosa): carcinoma invading submucosa, subdivided into:
– SM1: superficial invasion, ≤200 µm below MM
– SM2: deeper invasion into submucosa
As we know, JES vascular classification is based on the morphology of intraepithelial papillary capillary loops (IPCLs) observed by magnifying NBI endoscopy, allowing reliable prediction of invasion depth in squamous cell carcinoma of the esophagus (SSCC).
- Type A: normal or slightly irregular IPCLs, corresponding to inflammation or low-grade dysplasia (SIN)
- Type B1: small loop-like IPCLs appearing as dots under NBI → suggests superficial lesion T1a-EP/LPM
- Type B2: IPCLs lose loop structure, elongated and irregularly dilated → predicts T1a-MM or T1b-SM1 (invasion into MM or superficial SM)
- Type B3: markedly dilated IPCLs, >3× B2, often bluish → associated with T1b-SM2 or deeper, high nodal metastasis risk
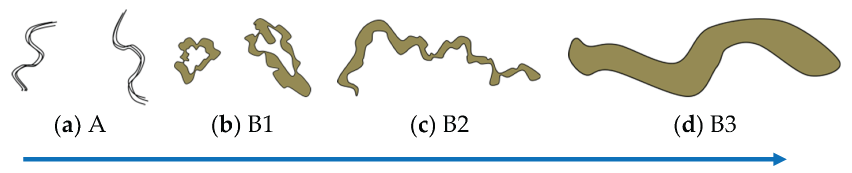
Correlation between JES classification and histopathology
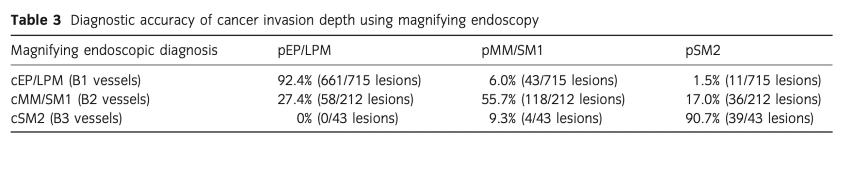
Studies show high accuracy in type B1 (92.4% = EP/LPM) and B3 (90.7% = SM2). However, type B2 represents a “gray zone,” with about 17% of actual cases invading SM2. Therefore, in this case, the doctor decided to perform EUS for further evaluation.
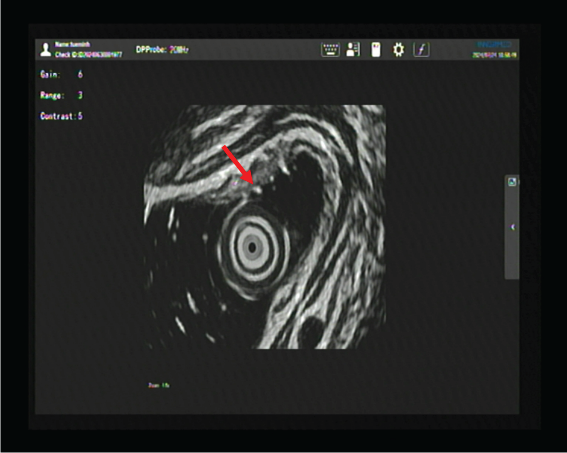
EUS results showed a hypoechoic lesion confined to the mucosal layer, while the submucosa remained relatively intact. Hence, ESD was chosen as the treatment strategy.
ESD procedure and outcome
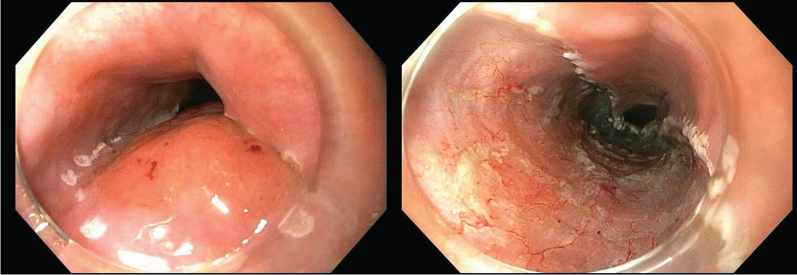
ESD procedure steps:
- Marking: Dual knife
- Submucosal injection: Non-lifting sign (-)
- Circumferential incision: Dual knife Cut 2, 30W
- Submucosal dissection: Dual knife Cut 2, 30W + Force coag 30W
- Hemostasis: Soft coag 40W
- Electrosurgical unit: Olympus ESG 100
- Total procedure time: 60 minutes
ESD outcome:
- Non-keratinizing squamous cell carcinoma, tumor invading lamina propria
- pT1a-LPM, v0, ly0, HM0, VM0
- Next step: Follow-up
Conclusion
This case highlights the critical role of JES classification in predicting invasion depth in esophageal squamous cell carcinoma. Clinical data show that type B1 and B3 patterns are usually accurate in depth prediction, while B2 is a gray zone requiring caution. Combining JES with EUS improves diagnostic accuracy and ensures safe ESD indication. The histopathological result of pT1a-LPM, without vascular invasion, with clear margins, and managed by follow-up only, demonstrates the value of a multimodal approach in modern esophageal endoscopy.