ENDOSTORY No.9: The First ESD Case – From Technical Trial to Strategic Intervention
For every medical facility, the first successful ESD case can represent a significant milestone—marking a major transition from the mucosal resection technique (EMR) to a deeper and more complex intervention with the potential for a more complete and effective curative treatment of early gastrointestinal cancer.
However, the process of transformation from a “technical trial” to an “effective intervention” requires that the practicing endoscopist not only master technical manipulations but also train extensively to gradually develop strategic interventional thinking.
Each ESD case is a sequence of strategic decisions—from lesion assessment, patient selection, and procedural planning to technical execution and complication management during and after the procedure.
ENDOSTORY #9 will take you through the process of developing strategic thinking in ESD, sharing practical experience distilled from many years of early cancer intervention by Dr. Tran Duc Canh, with the hope of offering practical insights to young endoscopists who are progressively mastering this technique.
Overview of the ESD technique
ESD (Endoscopic Submucosal Dissection) is an endoscopic technique for en bloc resection of submucosal gastrointestinal lesions, enabling treatment of large polyps, lesions suspected of malignant transformation, or early-stage malignant lesions.
Compared to EMR (Endoscopic Mucosal Resection), ESD has the advantage of en bloc removal even for difficult locations, allowing for accurate histopathological evaluation and reducing the risk of local recurrence.
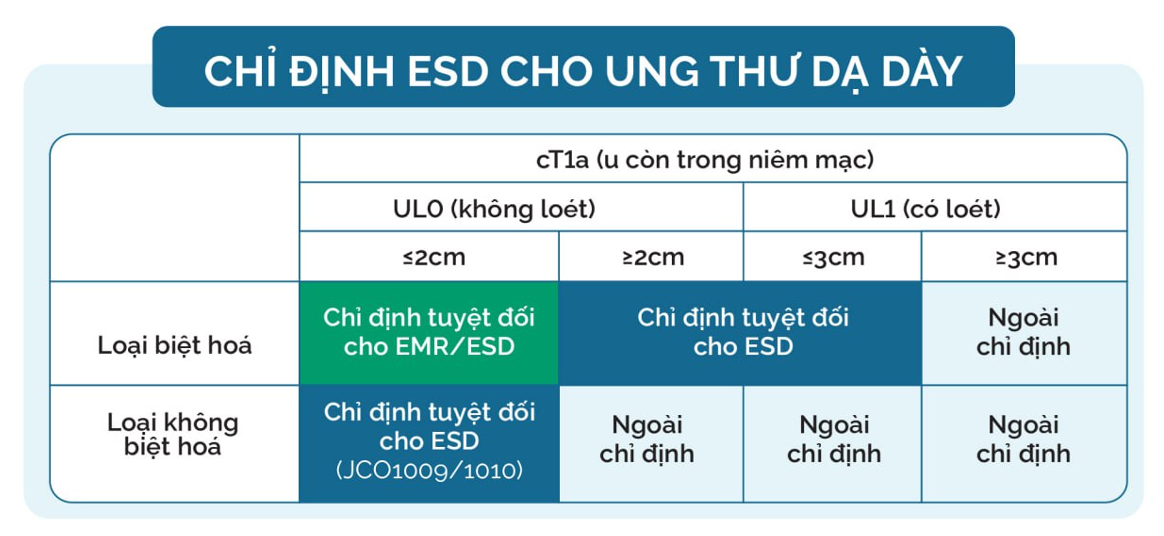
ESD is one of the standard treatments for early gastric cancer (cT1a)—when the tumor is still confined to the mucosa, has not invaded the muscularis mucosae or submucosa, and carries no risk of lymph node metastasis. According to JCOG1009/101, the indications for ESD in early gastric cancer are as follows:

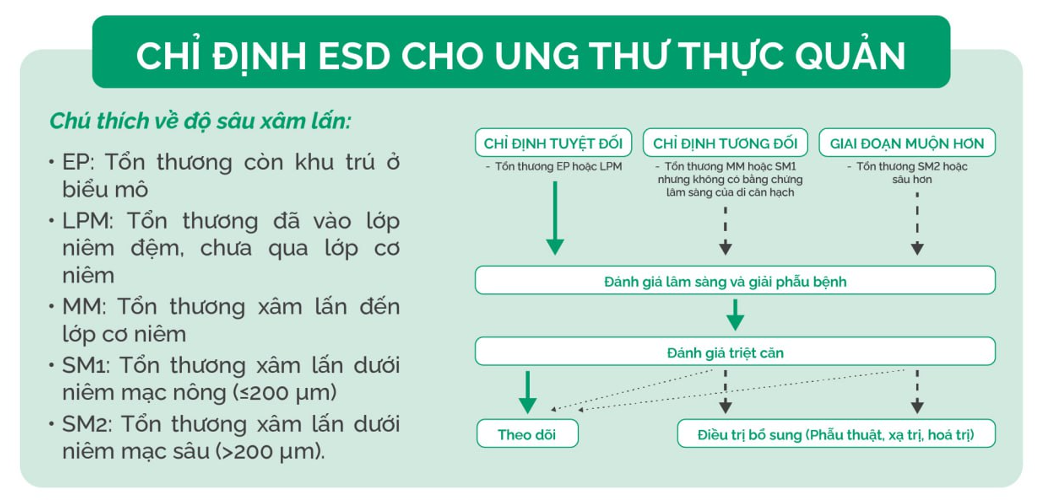
For esophageal lesions, ESD indications are determined by the depth of histological invasion and the risk of lymph node metastasis. The depth classification includes:
- EP (Epithelium): Lesion confined to the epithelial layer
- LPM (Lamina propria mucosae): Lesion invading the lamina propria, not beyond the muscularis mucosae
- MM (Muscularis mucosae): Lesion reaching the muscularis mucosae
- SM1: Superficial submucosal invasion (≤200 µm)
- SM2: Deep submucosal invasion (>200 µm)
According to JGES, the indications for esophageal lesions are summarized as follows:

Strategic thinking in ESD intervention
An effective ESD strategy does not begin with the first incision—it requires thorough preparation in theoretical knowledge, clinical assessment, and technical practice. This process can be structured into four main pillars:
Mastering theoretical knowledge: A fundamental foundation
To perform ESD safely and effectively, the endoscopist must be equipped with strong foundational knowledge. Classic references such as “Endoscopic Submucosal Dissection – Principles and Practice”, NBI atlases, and specialized books on Narrow Band Imaging serve as valuable educational resources.

Preoperative lesion assessment: Leave no detail overlooked
Assessment is typically performed 1–3 days prior to intervention, including:
- Lesion location (e.g., angularis minor, near pylorus, lower esophagus, etc.)
- Lesion size and surface morphology
- Suspected depth of invasion
- Risk of bleeding or perforation
- Risk of post-procedural stricture
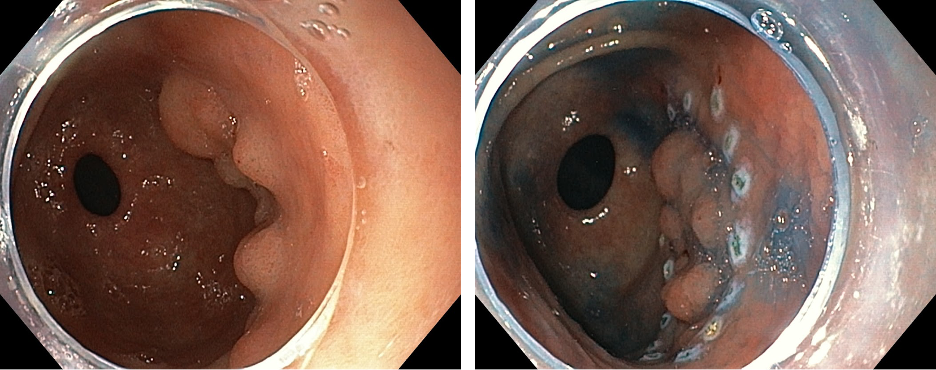
Advanced endoscopic techniques such as chromoendoscopy and magnifying NBI play a key role in identifying and evaluating lesions, thereby informing an appropriate resection strategy.
Evaluating procedural suitability: From an oncologist’s perspective
Not all lesions are suitable for ESD. Patient evaluation should comprehensively determine whether ESD is truly appropriate, considering factors such as:
- Treatment history: previous surgery, chemotherapy, or radiotherapy
- Comorbidities: coagulopathy, cardiac or respiratory conditions
- Clinical indication: whether ESD is genuinely necessary and appropriate
(Example: A patient with upper esophageal cancer near the orifice, stage T3N2 → Not suitable for ESD.)
Planning lesion resection and complication prevention
The interventional plan should be detailed, including:
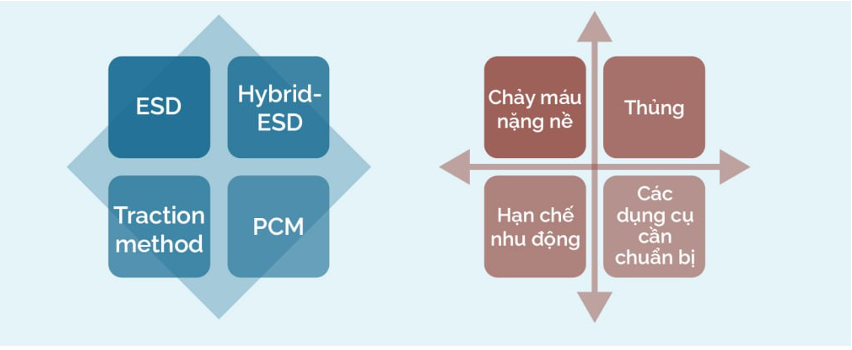
- Choice of technique: conventional ESD, hybrid ESD, traction method, or PCM (Pocket-creation method)
- Complication prevention strategy: preparation of hemostatic tools, control of perforation risk, and contingency plans for alternative approaches if difficulties arise
Additionally, the operator’s posture, monitor positioning, and coordination with assistants/nurses should be planned in advance to ensure a smooth procedure.
Practical experience from clinical practice
As one of the pioneers of ESD in Vietnam—having performed the country’s first ESD case in 2018—Dr. Tran Duc Canh shares several practical insights drawn from his extensive interventional endoscopy experience:
1.Approach strategies:
- Address difficult areas first, easier areas later.
Example: For a lesion at the angularis minor, start by incising the lesion margin near the angle using a DualKnife. - Approach fluid-dependent sides first.
Example: For esophageal lesions, inject the submucosa on the dependent side first and perform dissection from that side. Avoid injecting the opposite side first, as it can cause submucosal lifting and obscure access to the dependent side.
2. Knife selection depends on the operator’s preference. Dr. Canh typically uses ITKnife2 for gastric ESD and DualKnife or ITnano for esophageal ESD.
3. Use of ST Hood helps better access the submucosal layer and create a clear working field.

4. The optimal working posture is to stand upright with two monitors positioned directly in front and to the left of the endoscopist, minimizing fatigue during long procedures.
5. Practice the double-finger technique—using the left hand to control instruments—to perform faster and more precise maneuvers, reduce reliance on assistants, and maintain full control of the knife or hemostatic forceps.

6. Hold the endoscope shaft close to the body, resting it against the chest to maintain stability and minimize motion amplitude (different from ERCP or EUS handling).
7. There is no fixed rule regarding which foot should operate the electrosurgical pedal, but based on experience, using the left foot is preferable. The right foot can then control the water jet. Reason: The right hand always holds the scope or instrument—minimizing movement on the right side allows better control and stability when simultaneously dissecting and operating the pedal.
8. Bleeding prevention during ESD:
- Perform careful submucosal dissection
- Use active coagulation mode
- Avoid “blind cutting”; when visibility is poor, change the approach or use the hood to improve visualization
- Utilize RDI mode (integrated in the Olympus X1 system) to identify vessels and bleeding points accurately
9. Perforation prevention during ESD:
- Ensure adequate submucosal injection
- Avoid positioning the knife perpendicular to the muscularis layer
- Perform dissection with clockwise/counterclockwise scope rotation
- Use left/right-angle maneuvers proficiently
Conclusion
ESD is not only a proven minimally invasive therapeutic technique, but also a comprehensive test of strategic thinking, composure, and real-time decision-making ability.
Success does not begin when the knife touches the lesion—it starts much earlier, with patient assessment, strategic planning, and stepwise execution.
The experiences shared in this article do not replace clinical training but hopefully serve as a guiding framework for young endoscopists on their journey to mastering this meaningful and challenging technique.
About ENDOSTORY
ENDOSTORY is a clinical case-sharing series on practical gastrointestinal endoscopy, produced by Lenus Vietnam, aiming to provide valuable information for endoscopists. Each week, one “story” is selected and published on the Lenus Vietnam fanpage at 8:00 PM every Friday.
The series is scientifically supervised by Dr. Tran Duc Canh, an expert in early cancer diagnosis and treatment. Not only has Dr. Canh performed numerous complex ESD cases, but he has also trained many young Vietnamese endoscopists—helping to popularize this “golden key” technique in early gastrointestinal cancer treatment. His spirit of sharing and dedication has been a major inspiration for the creation of the ENDOSTORY journey.
As the program continues its early steps, we warmly welcome feedback for improvement. Please send your comments or discussions via Lenus Vietnam’s fanpage inbox or email [email protected] so we can listen and continue to refine the series.