[Endostory #10]: History of the formation & development of ESD – from polyp removal to the “EN-BLOC STANDARD” in gastrointestinal endoscopy
“If you want to go far, stand on the shoulders of giants” – this saying could not be more true when looking back on the journey of Endoscopic Submucosal Dissection (ESD). The sophisticated ESD cases we can perform today are the result of decades of research, creativity, and persistent refinement by generations of medical researchers.
The first step: The mission to remove the entire lesion
The journey of ESD began in the 1960s, when endoscopic polypectomy was first introduced [1,2]. From this starting point, researchers continued to search for solutions to remove larger lesions.
Around the 1980s to early 1990s in Japan, a series of endoscopic mucosal resection (EMR) variations emerged as minimally invasive treatment options for small early gastric cancers. These techniques included strip biopsy [3], endoscopic mucosal resection with local injection of hypertonic saline-epinephrine (ERHSE) [4,5], endoscopic double-snare polypectomy (EDSP) [6], and EMR with a cap-fitted panendoscope [7,8]. These improvements not only enhanced the safety and reliability of endoscopic interventions but also facilitated the worldwide adoption of EMR.
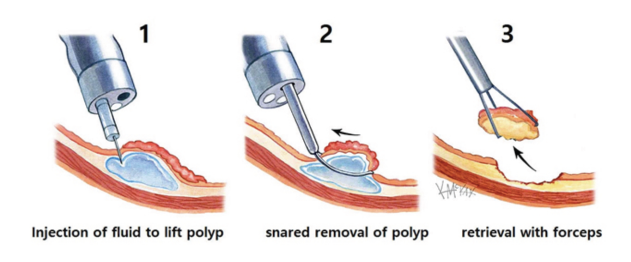
However, before the advent of ESD, ER techniques were limited by the size of the resectable specimen, which depended on the diameter of the snare or cap. Indications for ER at that time were mainly for lesions under 2 cm that could be resected en-bloc. Even for small lesions, the complete resection rate with EMR was under 70%, and incomplete or piecemeal resection increased the risk of local recurrence [9–11].
ESD was developed to overcome these limitations. With meticulous submucosal dissection, ESD enables en-bloc resection – removing the entire lesion with both lateral and deep margins intact. This approach adheres to surgical principles, isolates the lesion under direct endoscopic visualization, provides a whole specimen for accurate histological evaluation, and optimizes curability compared to piecemeal resection.
Thanks to its clear advantages, ESD was rapidly adopted for all parts of the gastrointestinal tract. Since 2006, Japan’s national health insurance has covered gastric–duodenal lesions, extending to the esophagus in 2008, and finally to the colorectum in 2012. Numerous studies, especially from East Asia, have shown that ESD increases R0 resection rates and reduces local recurrence compared to other endoscopic interventions [5,12–15].
A new height for ESD: The power of continuous innovation
ESD is characterized by two main steps: circumferential mucosal incision around the lesion and submucosal layer dissection.
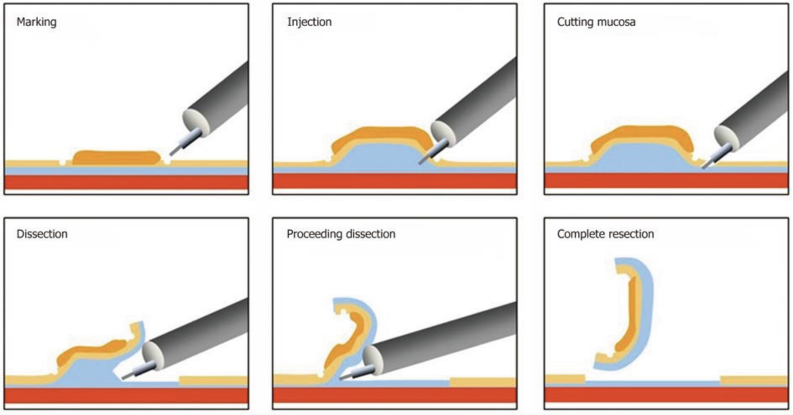
The idea of circumferential mucosal incision to preserve intact lateral margins dates back to EMR – specifically the ERHSE technique, where tissue removal was assisted by grasping forceps and a double-channel scope, similar to strip biopsy. Initially, mucosal incisions were made with a needle knife after injecting saline. However, with rudimentary knife tips, the needle knife often caused severe bleeding or perforation, preventing the technique from gaining widespread acceptance.
The turning point came with the advent of specialized ESD knives, enabling more precise and safer interventions. They can be classified into two main groups:
- Blunt-tip knives – Represented by the insulation-tipped (IT) knife developed by Hosokawa et al. [16–18]. With a hemispherical ceramic tip, the IT knife acts as a protective barrier to prevent deep cuts, controls blade mobility, and maintains a stable dissection speed.
- Cutting-tip knives – Allow multidirectional electrosurgical current from both the tip and blade edge, offering high flexibility but requiring careful observation and handling for safety. Many cutting-tip knives have thin, short cutting wires combined with an insulated sheath and distal stopper to control cutting depth and reduce the risk of deep injury. Examples include the Hook knife, Flex knife, Dual knife (Olympus), and Hybrid knife (ERBE).
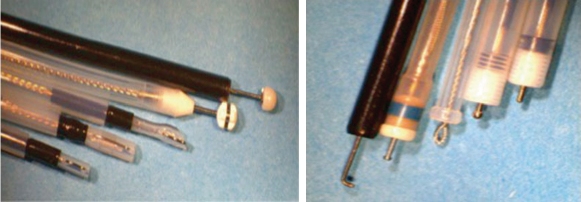
Along with knives, the electrosurgical unit (ESU) and current mode are crucial for success. The introduction of the EndoCut mode in ERBE generators enabled automatic adjustment of current intensity and cutting-coagulation characteristics depending on procedure stage, knife type, and target tissue. Cutting mode allows fast and precise dissection, while blended mode increases safety when dissecting vascular-rich submucosal tissue. Most bleeding during ESD can be immediately controlled with hemostatic forceps.
Creating a submucosal fluid cushion (SFC) is also a useful measure to prevent deep muscular injury during intervention, increasing procedural safety. For quick snare EMR, saline injection is sufficient, but prolonged ESD requires more stable solutions to protect the muscle layer. Many solutions have been tested, with hyaluronic acid (HA) – introduced by Yamamoto et al. [24–26] and later approved by Japan’s Ministry of Health, Labour and Welfare as a 0.4% injection (MUCOUP, Johnson & Johnson) – being notable. Outside Japan, cost-effective alternatives such as glycerol, dextrose, or hydroxypropyl methylcellulose (HPMC) [27–31] are also used due to their ability to maintain stable cushions.
To this day, researchers continue developing improved devices and injection solutions [32–36] to further enhance the efficacy and safety of ESD.
Challenges and future prospects
In Japan and many East Asian countries, ESD has become the first-line treatment for early gastrointestinal lesions, even for expanded indications such as large, differentiated intramucosal cancers without ulceration. Rigorous histological studies have shown ESD results equivalent to surgery in these cases.
However, acceptance of ESD varies worldwide. In Western countries, where early gastric cancer incidence is low, there is a shortage of suitable training cases (unlike the abundant Eastern data [12, 38, 39]), making it difficult to establish basic diagnostic and lesion-assessment skills. In challenging predicted endoscopic interventions, other methods – such as piecemeal resection or even surgery – may be considered.

New technology is opening possibilities: therapeutic endoscopes with triangular designs, dual movable instrument channels, or distal joint-control systems [40, 41] – enabling mucosal traction away from the dissection plane while using a needle knife for muscular dissection. Although still bulky, these systems are expected to be optimized for widespread future application.
Conclusion
ESD has revolutionized the management of early gastrointestinal lesions, enabling precise en-bloc resection with high curability. Over the past decade, alongside the development of instruments and technology, the technique has become increasingly refined and safe.
However, optimal outcomes require thorough endoscopist training – from diagnosis and patient preparation to post-procedure management. With ongoing technological progress, including robotic surgery, the prospect of ESD becoming a global standard for early GI lesion treatment is entirely realistic.
For young doctors, mastering ESD demands time and perseverance. But every successful case is not only a professional milestone but also a contribution to the legacy of this technique – a legacy written by the hands and hearts of today’s generation.
References
- Niwa H. Improvement of fibrogastroscope for biopsyand application of color television and high frequentcurrents for endoscopic biopsy (in Japanese).Gastroenterol Endosc. 1968;10:315.
- Tsuneoka K, Uchida T. Fibergastroscopic polypectomywith snare method and its significance developeding our department: polyp resection and recoveryinstruments (in Japanese with English abstract).Gastroenterol Endosc. 1969;11:174–84.
- Tada M, Shimada M, Murakami F, et al. Developmentof the strip-off biopsy [in Japanese with Englishabstract]. Gastroenterol Endosc. 1984;26:833–9.
- Hirao M, Masuda K, Asanuma T, et al. Endoscopicresection of early gastric cancer and other tumors withlocal injection of hypertonic saline-epinephrine.Gastrointest Endosc. 1988;34(3):264–9.
- Kakushima N, Fujishiro M. Endoscopic submucosaldissection for gastrointestinal neoplasms. World JGastroenterol. 2008;14(19):2962–7.
- Takekoshi T, Takagi K, Fujii A, et al. Treatment of earlygastric cancer by endoscopic double snare polypectomy(EDSP). Gan No Rinsho. 1986;32(10):1185–90.
- Inoue H, Takeshita K, Hori H, et al. Endoscopicmucosal resection with a cap-fi tted panendoscope foresophagus, stomach, and colon mucosal lesions.Gastrointest Endosc. 1993;39(1):58–62.
- Inoue H, Endo M, Takeshita K, et al. A new simplifi edtechnique of endoscopic esophageal mucosal resectionusing a cap-fi tted panendoscope (EMRC). SurgEndosc. 1992;6(5):264–5.
- Gossner L. The role of endoscopic resection and ablationtherapy for early lesions. Best Pract Res ClinGastroenterol. 2006;20(5):867–76.
- Sumiyama K, Gostout CJ. Novel techniques andinstrumentation for EMR, ESD, and full-thicknessendoscopic luminal resection. Gastrointest EndoscClin N Am. 2007;17(3):471. 85, v–vi.
- Gotoda T. Endoscopic resection of early gastric cancer.Gastric Cancer.2007;10(1):1–11.
- Draganov PV, Gotoda T, Chavalitdhamrong D, et al.Techniques of endoscopic submucosal dissection:application for the Western endoscopist? GastrointestEndosc. 2013;78(5):677–88.
- Toyonaga T, Man-i M, East JE, et al. 1,635 Endoscopicsubmucosal dissection cases in the esophagus, stomach,and colorectum: complication rates and longtermoutcomes. Surg Endosc. 2013;27(3):1000–8.
- Toyonaga T, Man-i M, Chinzei R, et al. Endoscopictreatment for early stage colorectal tumors: the comparisonbetween EMR with small incision, simplifi ed ESD,and ESD using the standard fl ush knife and the balltipped fl ush knife. Acta Chir Iugosl. 2010;57(3):41–6.
- Tanabe S, Ishido K, Higuchi K, et al. Long-term outcomesof endoscopic submucosal dissection for earlygastric cancer: a retrospective comparison with conventionalendoscopic resection in a single center.Gastric Cancer. 2014;17:130.
- Ohkuwa M, Hosokawa K, Boku N, et al. New endoscopictreatment for intramucosal gastric tumorsusing an insulated-tip diathermic knife. Endoscopy.2001;33(3):221–6.
- Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosalresection for treatment of early gastric cancer. Gut.2001;48(2):225–9.
- Hosokawa KYS. Recent advances in endoscopicmucosal resection for early gastric cancer [Japanese].Gan To Kagaku Ryoho. 1998;25:476–83.
- Oyama T, Tomori A, Hotta K, et al. Endoscopic submucosaldissection of early esophageal cancer. ClinGastroenterol Hepatol. 2005;3(7 Suppl 1):S67–70.
- Yahagi N, Fujishiro M, Kakushima N, et al.Endoscopic submucosal dissection for early gastriccancer using the tip of an electrosurgical snare (thintype). Dig Endosc.2004;16:34–6.
- Yahagi N, Neuhaus H, Schumacher B, et al. Comparisonof standard endoscopic submucosal dissection (ESD)versus an optimized ESD technique for the colon: ananimal study. Endoscopy. 2009;41(4):340–5.
- Toyonaga T, Man-I M, Fujita T, et al. The performanceof a novel ball-tipped Flush knife for endoscopicsubmucosal dissection: a case-control study.Aliment Pharmacol Ther. 2010;32(7):908–15.
- Neuhaus H, Wirths K, Schenk M, et al. Randomizedcontrolled study of EMR versus endoscopic submucosaldissection with a water-jet hybrid-knife of esophageallesions in a porcine model. Gastrointest Endosc.2009;70(1):112–20.
- Yamamoto H, Yahagi N, Oyama T, et al. Usefulnessand safety of 0.4% sodium hyaluronate solution as asubmucosal fluid “cushion” in endoscopic resectionfor gastric neoplasms: a prospective multicenter trial.Gastrointest Endosc. 2008;67(6):830–9.
- Yamamoto H, Yube T, Isoda N, et al. A novel methodof endoscopic mucosal resection using sodium hyaluronate.Gastrointest Endosc. 1999;50(2):251–6.
- Yamamoto H, Koiwai H, Yube T, et al. A successfulsingle-step endoscopic resection of a 40 millimeterflat-elevated tumor in the rectum: endoscopic mucosalresection using sodium hyaluronate. GastrointestEndosc. 1999;50(5):701–4.
- Fujishiro M, Yahagi N, Kashimura K, et al. Tissuedamage of different submucosal injection solutionsfor EMR. Gastrointest Endosc. 2005;62(6):933–42.
- Fujishiro M, Yahagi N, Kashimura K, et al. Comparisonof various submucosal injection solutions for maintainingmucosal elevation during endoscopic mucosalresection. Endoscopy. 2004;36(7):579–83.
- Fujishiro M, Yahagi N, Kashimura K, et al. Differentmixtures of sodium hyaluronate and their ability tocreate submucosal fl uid cushions for endoscopicmucosal resection. Endoscopy. 2004;36(7):584–9.
- Conio M, Rajan E, Sorbi D, et al. Comparative performancein the porcine esophagus of different solutionsused for submucosal injection. Gastrointest Endosc.2002;56(4):513–6.
- Feitoza AB, Gostout CJ, Burgart LJ, et al.Hydroxypropyl methylcellulose: a better submucosalfluid cushion for endoscopic mucosal resection.Gastrointest Endosc. 2003;57(1):41–7.
- Sumiyama K, Gostout CJ, Rajan E, et al. Chemicallyassisted endoscopic mechanical submucosal dissectionby using mesna. Gastrointest Endosc. 2008;67(3):534–8.
- Sumiyama K, Tajiri H, Gostout CJ, et al. Chemicallyassisted submucosal injection facilitates endoscopicsubmucosal dissection of gastric neoplasms.Endoscopy. 2010;42(8):627–32.
- Sumiyama K, Toyoizumi H, Ohya TR, et al. A doubleblind,block-randomized, placebo-controlled trial toidentify the chemical assistance effect of mesna submucosalinjection for gastric endoscopic submucosaldissection. Gastrointest Endosc. 2014;79:756.
- Chandrasekhara V, Sigmon Jr JC, Surti VC, et al. Anovel gel provides durable submucosal cushion forendoscopic mucosal resection and endoscopic submucosaldissection. Surg Endosc. 2013;27(8):3039–42.
- Khashab MA, Saxena P, Sharaiha RZ, et al. A novelsubmucosal gel permits simple and effi cient gastricendoscopic submucosal dissection. Gastroenterology.2013;144(3):505–7.
- Gotoda T, Iwasaki M, Kusano C, et al. Endoscopicresection of early gastric cancer treated by guidelineand expanded National Cancer Centre criteria. Br JSurg. 2010;97(6):868–71.
- Draganov PV, Coman RM, Gotoda T. Training forcomplex endoscopic procedures: how to incorporateendoscopic submucosal dissection skills in the West?Expert Rev Gastroenterol Hepatol. 2014;8:119.
- Schumacher B, Charton JP, Nordmann T, et al.Endoscopic submucosal dissection of early gastric neoplasiawith a water jet-assisted knife: a Western, singlecenterexperience. Gastrointest Endosc. 2012;75(6):1166–74.
- Ikeda K, Sumiyama K, Tajiri H, et al. Evaluation of anew multitasking platform for endoscopic fullthicknessresection. Gastrointest Endosc. 2011;73(1):117–22.
- Yonezawa J, Kaise M, Sumiyama K, et al. A noveldouble-channel therapeutic endoscope (“R-scope”)facilitates endoscopic submucosal dissection of superficial gastric neoplasms. Endoscopy. 2006;38(10):1011–5.
- Ho KY, Phee SJ, Shabbir A, et al. Endoscopic submucosaldissection of gastric lesions by using a Masterand Slave Transluminal Endoscopic Robot(MASTER). Gastrointest Endosc. 2010;72(3):593–9.
- Phee SJ, Reddy N, Chiu PW, et al. Robot-assistedendoscopic submucosal dissection is effective in treatingpatients with early-stage gastric neoplasia. ClinGastroenterol Hepatol. 2012;10(10):1117–21.
About ENDOSTORY
ENDOSTORY is a clinical gastroenterology endoscopy case-sharing series produced by Lenus Vietnam, aiming to provide useful information for endoscopists. Each week, a “story” is selected and posted on the Lenus Vietnam fanpage at 8:00 p.m. on Friday.
The series is medically advised by Dr. Tran Duc Canh – an expert in early cancer diagnosis and treatment. Not only has Dr. Canh personally performed numerous complex ESD cases, but he has also trained many young Vietnamese endoscopists in ESD, contributing to the widespread adoption of this “golden key” technique for early GI cancer treatment. His spirit of sharing and dedication is part of the inspiration behind the creation of the “endoscopy storytelling” journey that is ENDOSTORY.