ENDOSTORY #8: BROWNISH AREA IN THE ESOPHAGUS – SIGN OF MALIGNANCY OR JUST A “FALSE ALARM”?
In esophageal endoscopy using NBI (Narrow Band Imaging), a brownish area (BA) is a commonly encountered visual finding that can cause diagnostic uncertainty: it may be an early indicator of squamous cell carcinoma, but it can also be a pseudo-lesion caused by mucosal peeling, epithelial atrophy, or nonspecific changes. Follow this ENDOSTORY case #8 to see how the physician managed the brownish area to accurately determine the nature of the lesion and make a timely and appropriate diagnosis.
Case Information
A 62-year-old male patient with a history of colon cancer stage pT2N0M0. After treatment, he underwent annual surveillance endoscopy. In a recent follow-up, a suspicious mucosal lesion was found in the esophagus.
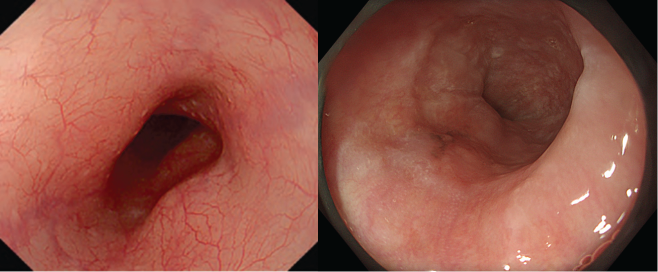
Initial analysis using White Light Imaging (WLI)
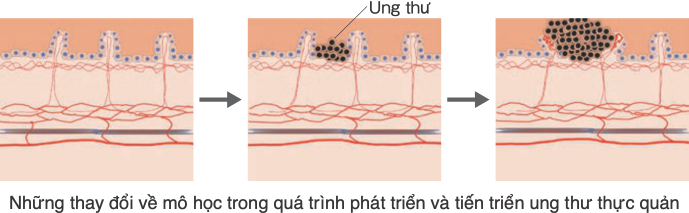
Under white light (WLI), normal esophageal mucosa appears smooth and glossy, with visible branching vessels in the deeper layers. In early esophageal cancer, the tumor originates from the basal layer and gradually proliferates, replacing the basal cells of the epithelium. As cellular density increases, the transparency of the epithelium decreases, making subepithelial vessels less visible and changing the mucosal color to a more reddish hue.
Thus, WLI allows for the prediction of hyperplastic areas based on changes in color and mucosal surface topography. Keratinized lesions can also be identified by white, granular-appearing material on the mucosal surface. However, in very early esophageal lesions, subtle differences in mucosal glossiness must be carefully noted.
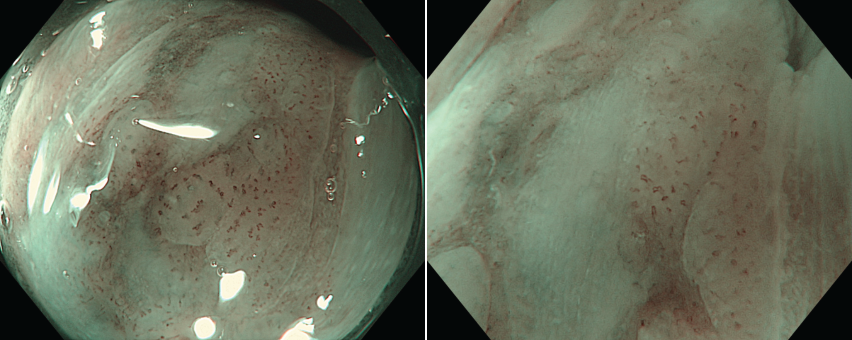
In this case, WLI showed a lesion classified as Paris type 0-IIc, approximately 20 mm in size, located in the lower thoracic esophagus, with a slightly reddish hue, well-defined borders, and no ulceration.
Brownish areas: when are they malignant, and when are they just “false alarms”?
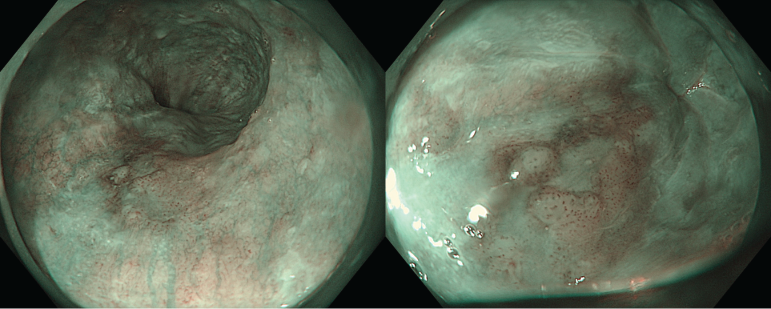
Upon switching to NBI mode, brownish areas (BAs) were observed at a distance.
A brownish area (BA) refers to a section of esophageal mucosa that appears darker than the surrounding tissue under NBI, especially at a distant view. BAs result from two main factors: abnormal blood vessels (e.g., proliferation, dilation, deformation) and darkened mucosal background coloration.
While not specific for cancer, BAs strongly suggest abnormal lesions, especially early esophageal squamous cell carcinoma (ESCC). However, in cases of epithelial atrophy (also called “false brown areas”), thin squamous epithelium or mucosal peeling caused by the endoscope may also alter mucosal coloration. Therefore, magnified NBI is essential for evaluating whether a BA is truly malignant.
Magnified NBI and the role of JES classification in assessing invasion depth
Esophageal squamous cell carcinoma typically originates from basal cells in the deepest epithelial layer. Normally, these cells are aligned along the basement membrane, then gradually differentiate and move toward the surface, forming stratified squamous epithelium.
In early stages, tumors proliferate within the epithelial layer, sometimes retaining a normal-looking surface under WLI. As proliferation continues, the tumor thickens, creating raised or depressed lesions and invading beneath the basement membrane. Surface keratinization, not seen in normal esophageal epithelium, may also occur.
The esophageal squamous epithelium contains a characteristic vascular structure called IPCL (intra-epithelial papillary capillary loop). These capillaries are the size of red blood cells and loop from the submucosa to the surface. When a lesion proliferates, IPCLs become distorted, lose their loop shape, are displaced by the tumor, or disappear altogether. This forms the basis of the JES classification.
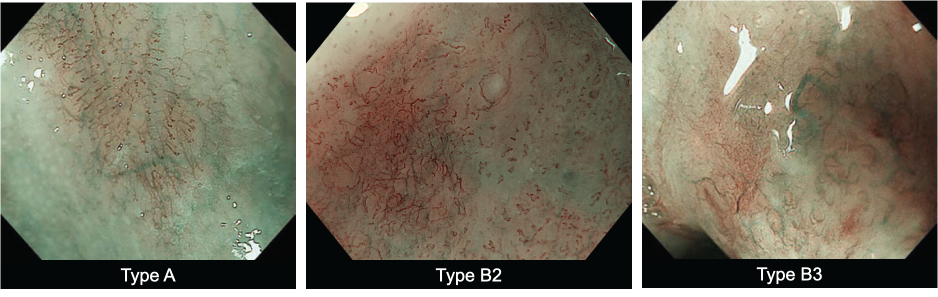
The Japan Esophageal Society (JES) classifies IPCLs into 4 main types and an additional avascular area (AVA) category, with corresponding predictions for invasion depth:
| Type | IPCL Characteristics | Predicted Invasion Depth |
| A | No or slight changes in IPCL | Non-cancerous / SIN |
| B1 | Abnormal loop-shaped vessels showing dilation, tortuosity, irregular caliber & shape | EP/LPM (superficial) |
| B2 | Abnormal vessels with few loop formations | MM/SM1 (shallow submucosal) |
| B3 | Markedly dilated, irregular vessels (2x size of B2) | SM2 or deeper (deep invasion) |
| AVA-small | <0.5 mm | EP/LPM |
| AVA-middle | ≥0.5 mm to <3 mm | MM/SM1 |
| AVA-large | ≥3 mm | SM2 or deeper |
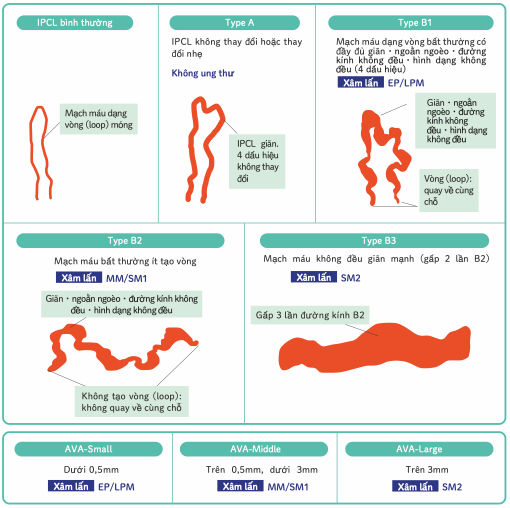
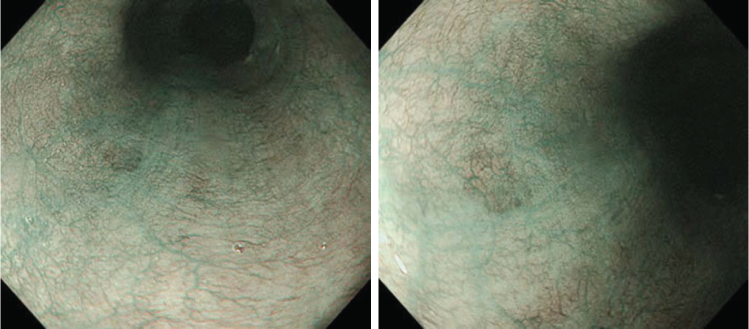
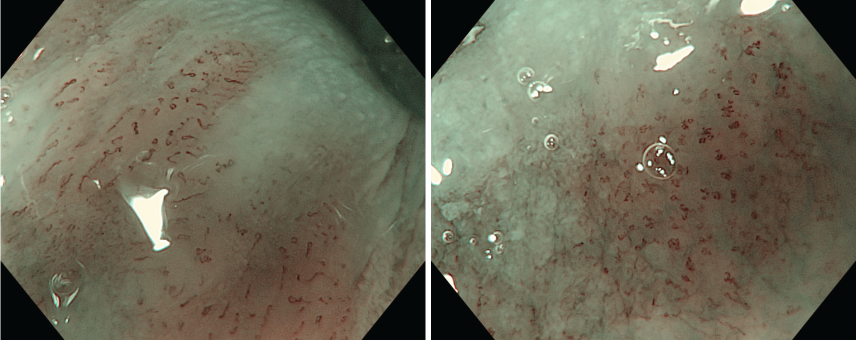
In this case, magnified NBI revealed IPCLs with all four abnormal features (dilation, tortuosity, irregular caliber, irregular shape), classifying the lesion as Type B1 – indicating superficial invasion.
Note: Biopsy showing only SIN (squamous intraepithelial neoplasia)
Even when endoscopic imaging strongly suggests cancer, histology may only indicate dysplasia (SIN), without confirming malignancy. This discrepancy may be due to biopsy errors—sampling the dysplastic periphery of a cancerous lesion or obtaining too few cancerous cells for a histologic diagnosis.
Some studies suggest that magnified NBI can match biopsy in diagnostic accuracy for ESCC (1). Thus, if endoscopic findings strongly suggest malignancy, endoscopic treatment (e.g., ESD) may be performed as a diagnostic therapy. Conversely, if the lesion is not suspicious, follow-up endoscopy in 6–12 months is recommended.
Conclusion
Biopsy confirmed the lesion as squamous cell carcinoma (SCC). Based on imaging and biopsy, the lesion was considered very early stage (Tis–T1a), measuring 15 mm, with high-grade dysplasia (HGD). According to current guidelines, this lesion met absolute indications for ESD.
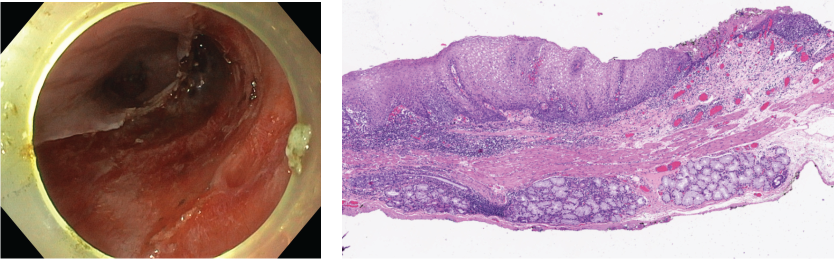
After ESD and histopathology, the final diagnosis was: in-situ squamous cell carcinoma (pTis), no lymphovascular invasion (ly0, v0), and negative horizontal and vertical margins (HM0, VM0).