ENDOSTORY No.14: Expanded ESD Indication for a Large Early Gastric Cancer Lesion
In the treatment of early gastric cancer, absolute indications for ESD have become common for small lesions ≤ 2 cm in size, with an almost zero risk of lymph node metastasis, no ulceration (UL0), and confined to the mucosal layer (T1a). In contrast, expanded indications for ESD, which apply to larger lesions, require more extensive observation and assessment based on magnifying endoscopy as well as thorough histopathological evaluation after intervention.
This week, ENDOSTORY #14 presents a clinical case featuring a lesion > 3 cm under the expanded ESD indication, along with detailed evaluations before and after the ESD procedure performed by the physician.
Clinical presentation and paraclinical evaluations
A 61-year-old male patient with no significant medical history was admitted with complaints of prolonged abdominal pain, without vomiting or weight loss. On examination, a gastric mass was detected.
Blood tests showed elevated liver enzymes (GOT, GPT) and uric acid levels, while abdominal ultrasound revealed no abnormalities. Gastroscopy identified a lesion at the gastric body, along the greater curvature and posterior wall, classified as type 0-IIa+c, approximately 4 cm in size, with clear margins. Initial histopathology revealed high-grade dysplasia.
Evaluation according to the Kyoto classification, with a total score of 5, indicated a very high risk of gastric cancer, based on the following findings:
- Atrophic border (C-O: C2): 1 point
- Intestinal metaplasia: 1 point
- Enlarged gastric folds: 1 point
- Nodularity: 0 points
- Diffuse redness, RAC (–): 2 points
- HP positive
=> Total score: 5
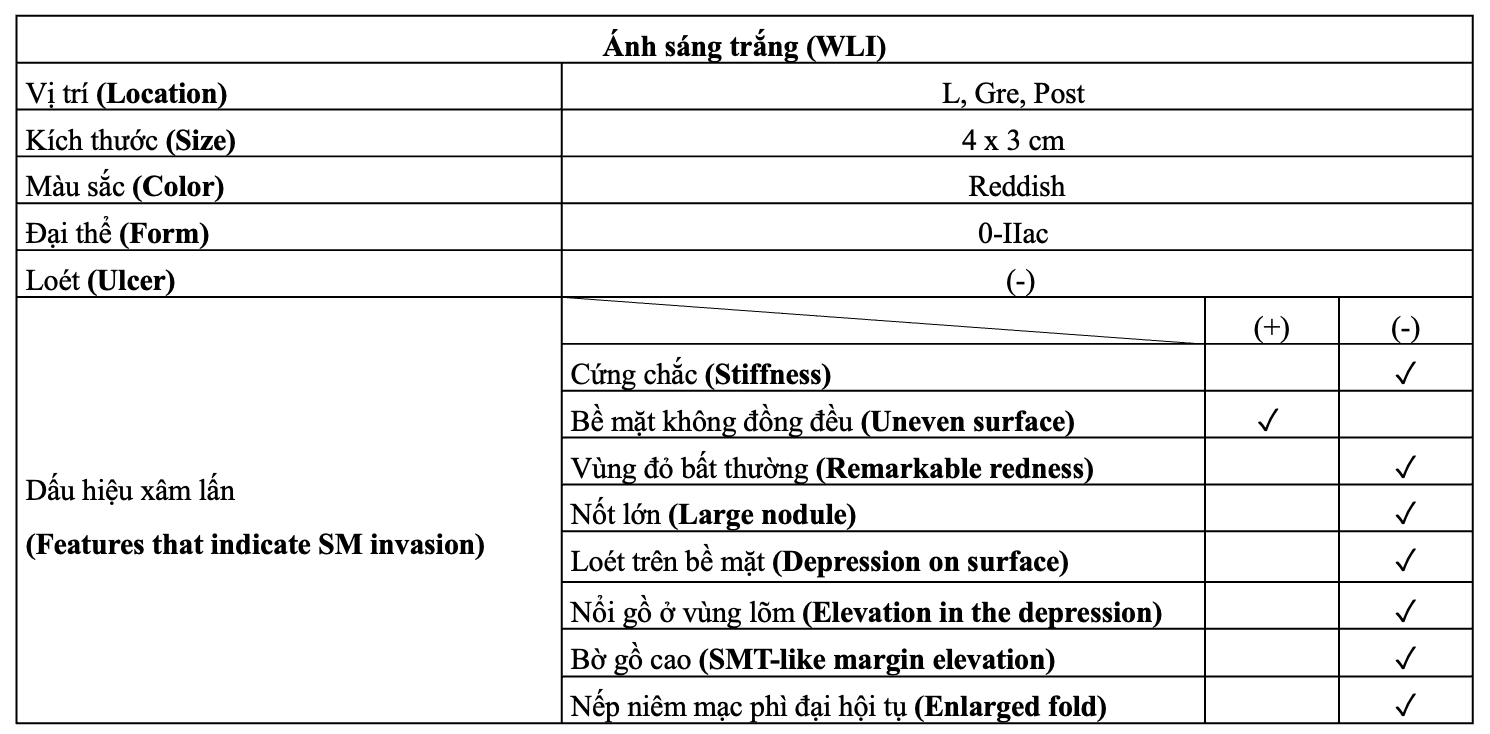
Lesion evaluation under WLI (White Light Imaging)
The lesion was located at the gastric body, greater curvature, posterior wall (L, Gre, Post), measuring approximately 4 × 3 cm, morphology 0-IIa+c, dark reddish in color. Notably, no ulceration was observed.
Among the indicators suggestive of submucosal (SM) invasion, the only positive sign was an uneven surface pattern.
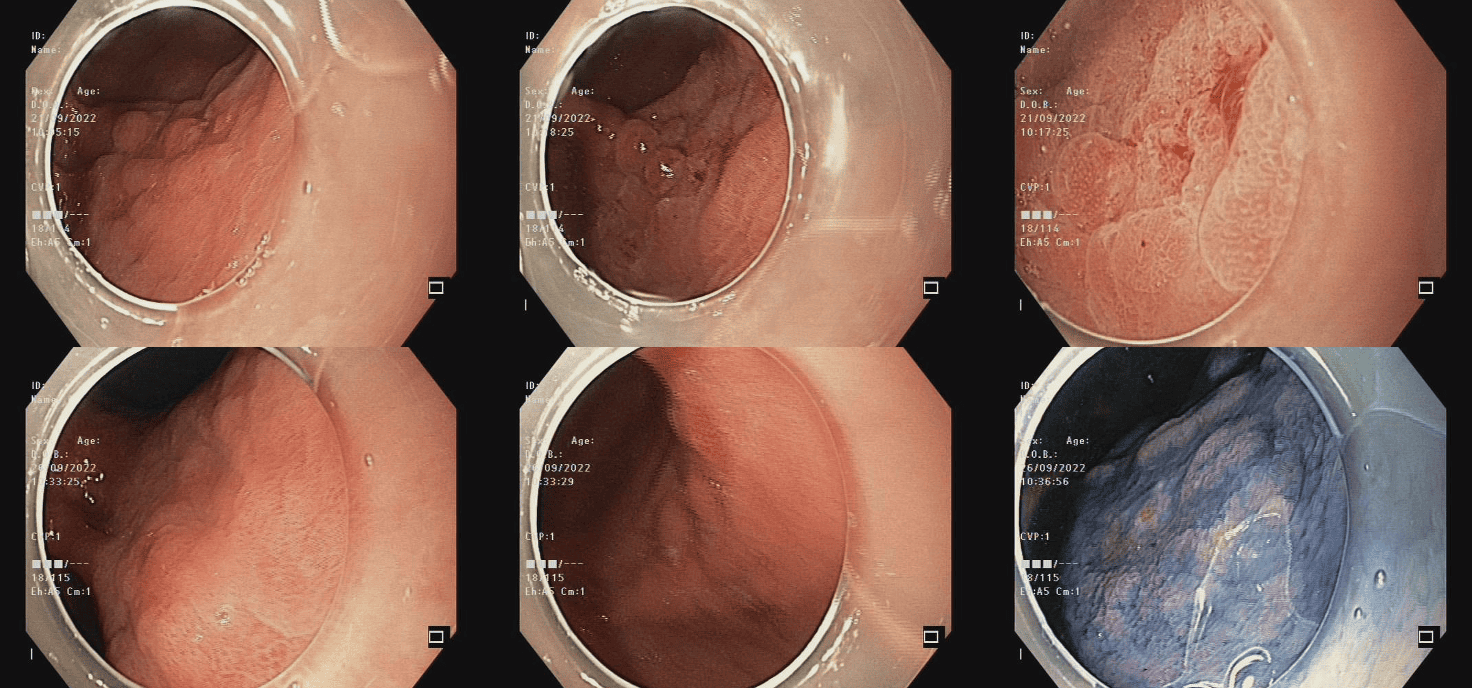
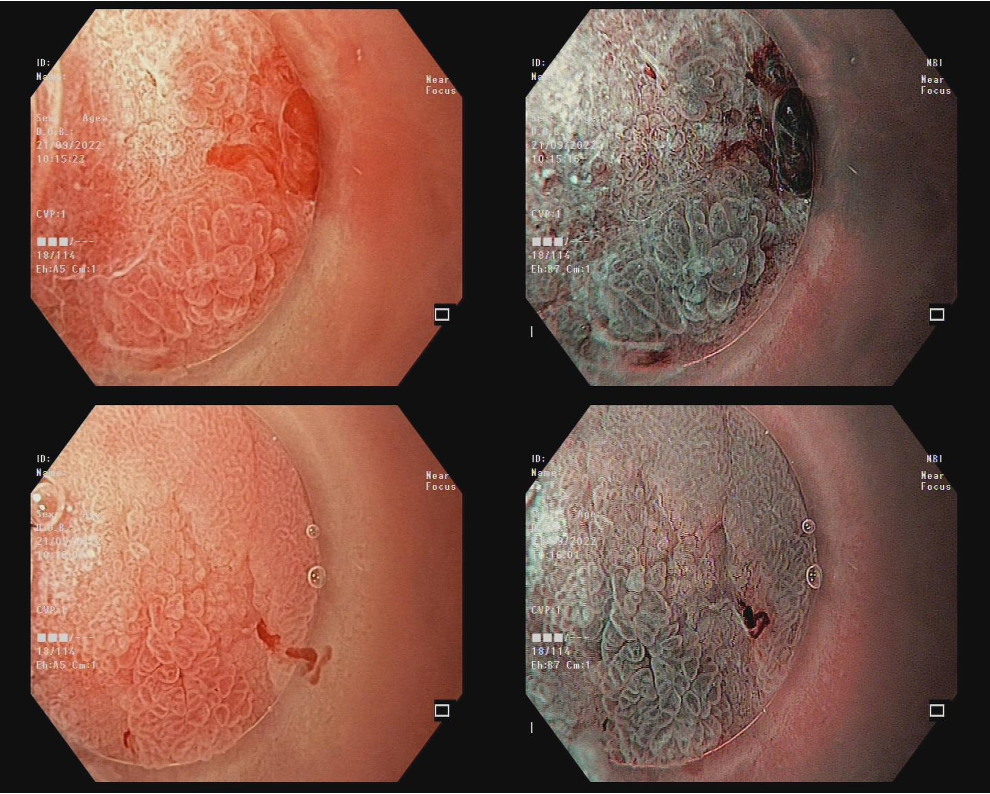
Evaluation on magnifying NBI: background mucosa, marginal area, lesion mucosa, and other related findings
On magnifying NBI images, the micro-surface (MS) and microvascular (MV) structures of the background mucosa were preserved, showing normal characteristics. The microvessels were symmetrically distributed and regularly arranged, while the marginal crypt epithelium displayed uniform oval or crescent shapes.
Of note, LBC (+) (Light Blue Crest) was present — a typical feature suggesting intestinal metaplasia. However, no structural or vascular irregularity was observed.
This indicates that the background mucosa exhibited chronic changes (intestinal metaplasia) but did not show any evidence of severe dysplasia or malignancy beyond the main lesion area.

Evaluation of the margin revealed a well-defined demarcation line and signs of intraepithelial microinvasion.

Observation of the lesion mucosa showed significant alterations in both MV and MS structures. The microvasculature appeared irregular, tortuous, and dilated, while the epithelial surface structure was deformed and lost its original uniformity.

In addition, irregular and asymmetrically distributed WOS (white opaque substance) was observed — another sign suggestive of malignancy.

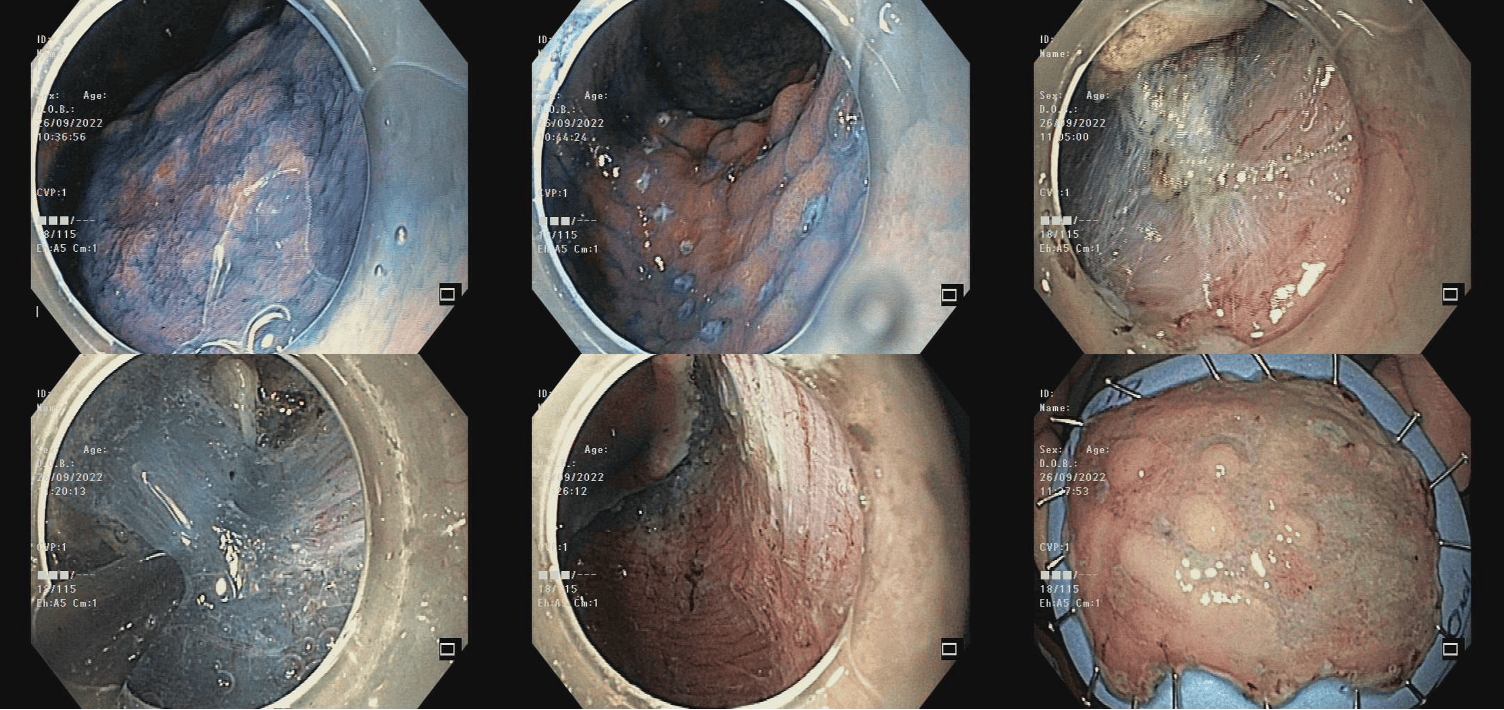
Expanded indication for ESD
Based on detailed evaluation under magnifying endoscopy, the lesion demonstrated clear demarcation, irregular vascular distribution, and heterogeneous mucosal surface — all strongly suggestive of malignancy.
- Diagnosis: Gastric adenocarcinoma (carcinoma)
- Predicted invasion depth: T1a, limited from the lamina propria (LPM) to the muscularis mucosae (MM)
- Predicted histology: Well-differentiated adenocarcinoma (WDA)
Treatment plan
- Lesion size > 3 cm
- Well-differentiated histology
- Stage T1a
With these characteristics, the patient was indicated for expanded ESD.
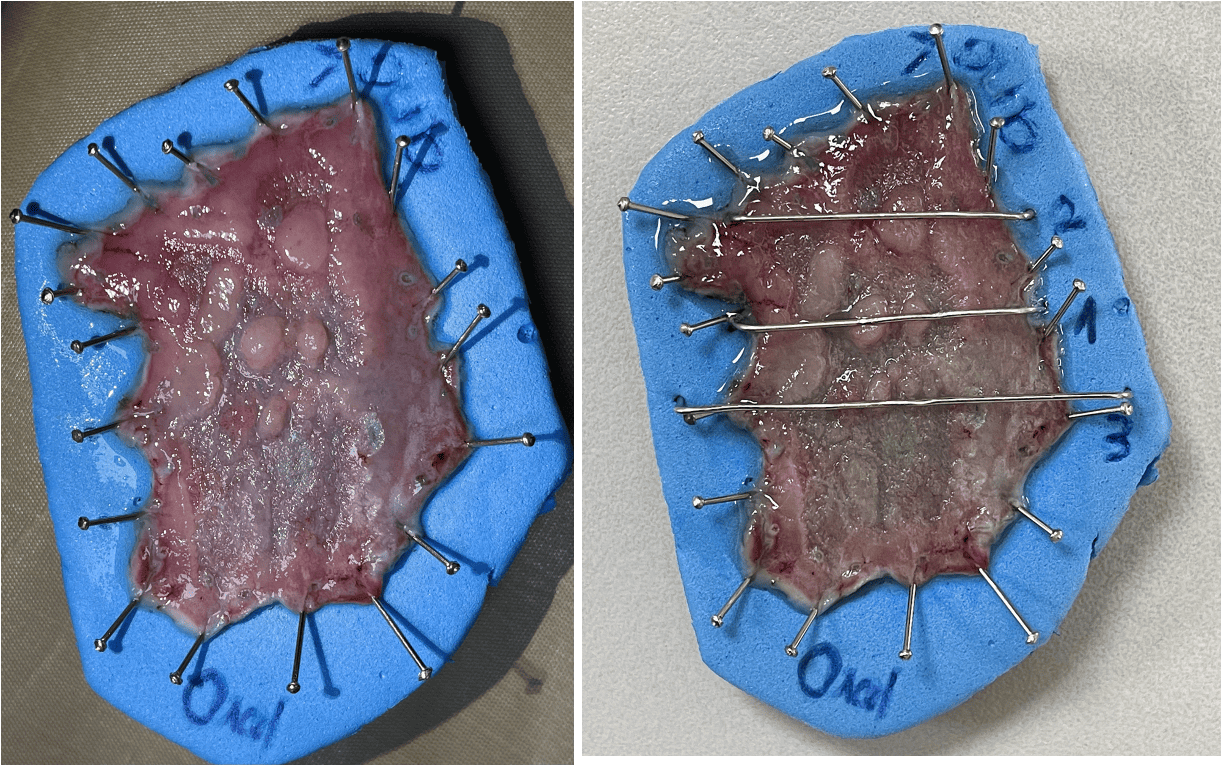
Outcome: The ESD procedure was completed within 50 minutes, with no intra- or post-procedural complications.
Histopathological evaluation
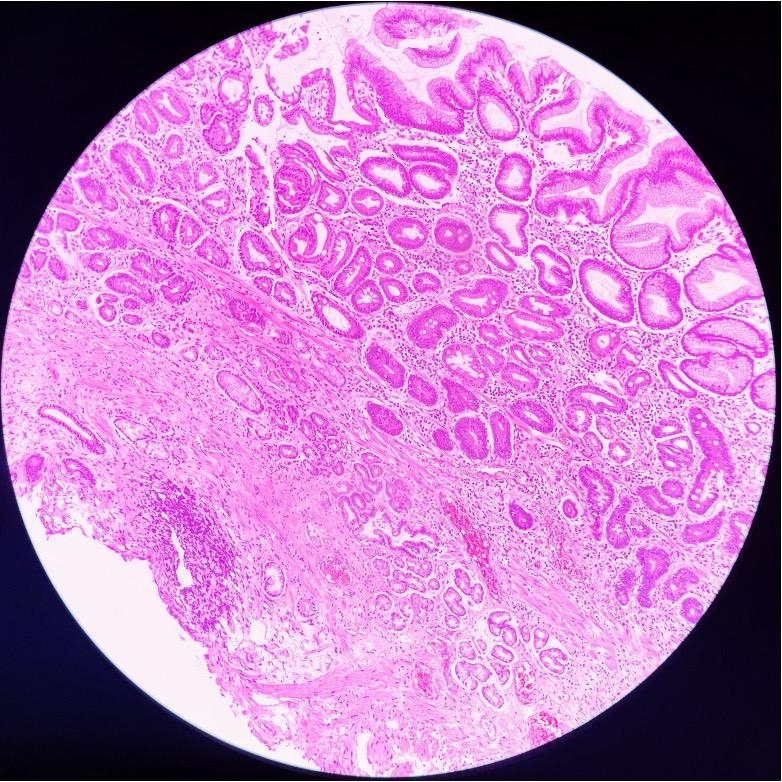
Examination of three histological sections revealed the following:
Sections 1 and 2:
- The surface glandular epithelium showed low-grade dysplasia with preserved structural uniformity; the marginal (depressed) epithelium appeared atrophic, carcinoma.
- The lamina propria exhibited infiltration of numerous inflammatory cells.
- The muscularis mucosae (MM) and submucosa (SM) remained intact.
- Goblet cells were present.
Section 3:
- Surface glandular epithelium with low-grade dysplasia.
- Lamina propria with marked inflammatory cell infiltration.
- MM and SM structures remained intact.
Across all three sections, histology showed chronic gastritis with localized inflammatory cell infiltration forming small cystic spaces in the lamina propria. This phenomenon led to elevation of the lamina propria, resulting in surface epithelial protrusion.

Within the cancerous area, histological findings demonstrated clear malignant transformation compared with the inflammatory mucosal sections. The surface epithelium and glandular architecture had markedly changed: tumor cells exhibited hyperchromatic nuclei, disorganized arrangement, loss of polarity, and absence of distinct mucinous vacuoles.
The neoplastic glands appeared crowded, forming cribriform or back-to-back patterns, creating clusters of abnormal glands. Importantly, cancer cells had breached the basement membrane and invaded the lamina propria, confirming the diagnosis of gastric adenocarcinoma.
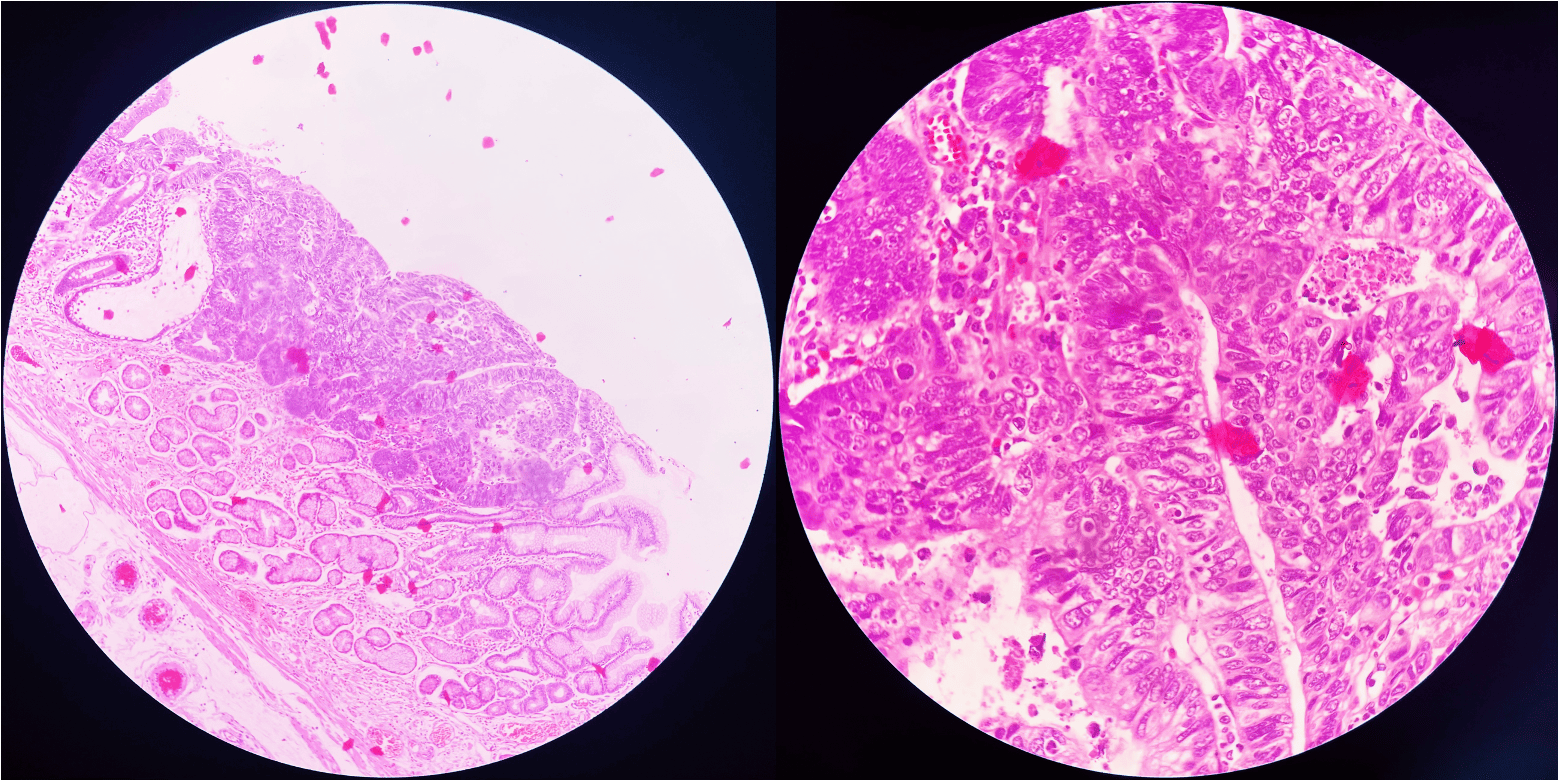
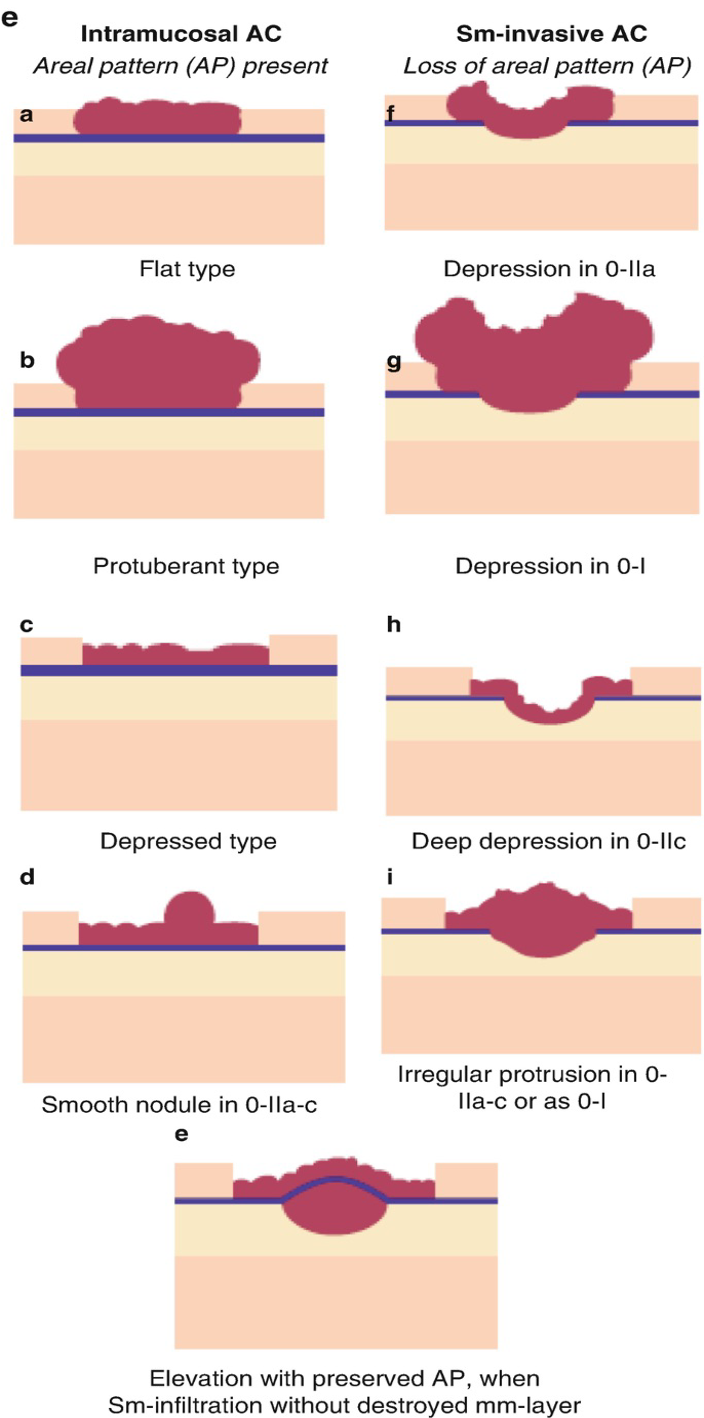
An important aspect in the assessment of early gastric cancer is predicting the invasion depth based on lesion morphology — distinguishing between intramucosal adenocarcinoma (AC) and submucosal invasive AC (SM-invasive AC).
- For intramucosal lesions, the characteristic feature is the preservation of the areal pattern (AP). Common morphologies include flat, slightly elevated, mildly depressed, or nodular lesions.
- In contrast, when invasion extends into the submucosa, the AP tends to be disrupted, and the surface becomes irregular, with deep depression (0-IIc), uneven elevation, or a combined depressed–elevated appearance. These are significant indicators suggesting SM invasion and carry important prognostic implications.
In this case, histopathological examination confirmed that the carcinoma was confined to the mucosal layer (T1a-MM), consistent with the 0-IIa+c morphology observed endoscopically. This finding not only reinforces the reliability of endoscopic assessment but also validates that the choice of expanded ESD was both appropriate and safe.