Endostory No.16: Indentifying metachronous cancer during postoperative follow-up after esophageal surgery
In clinical practice, follow-up for patients after esophageal cancer surgery presents multiple challenges—not only the risk of recurrence but also the possible emergence of new malignant lesions, known as metachronous cancer. Although differentiating between the two is not always straightforward, it plays a crucial role in diagnosis and treatment decisions.
The case presented in EndoStory #16 involves a patient who had previously undergone esophagogastric resection and developed a new lesion more than one year later. Is this a recurrence or a new primary tumor? And what is the appropriate management?
Case Presentation
The patient in EndoStory #16 is a 62-year-old male with a history of esophagogastric resection and reconstruction performed in July 2024. Postoperatively, he was followed up regularly. In August 2025, during a routine examination, a new abnormal lesion was detected. Biopsy confirmed invasive squamous cell carcinoma (SCC).
Blood count and biochemical tests were within normal limits. PET-CT revealed thickening at the esophagogastric anastomosis and mildly increased FDG uptake in the upper one-third of the esophagus.
Observation under White Light and NBI
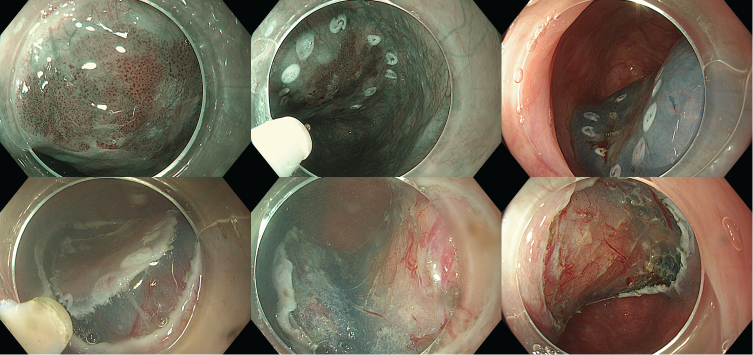
Under white light imaging (WLI), the esophagogastric anastomosis was observed approximately 20 cm from the upper incisors, showing smooth mucosa and good anastomotic patency. However, at 17–18 cm from the incisors, a slightly elevated reddish lesion (approximately 15 mm) was seen, corresponding to a type 0-IIa superficial lesion.
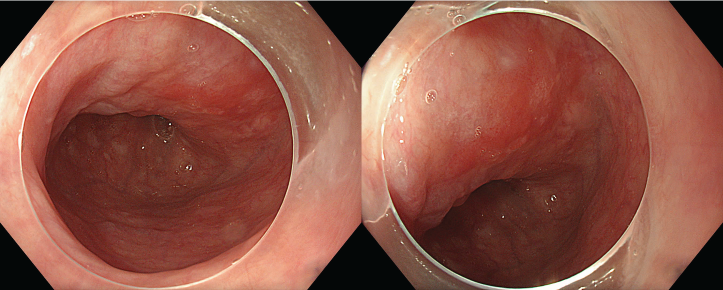
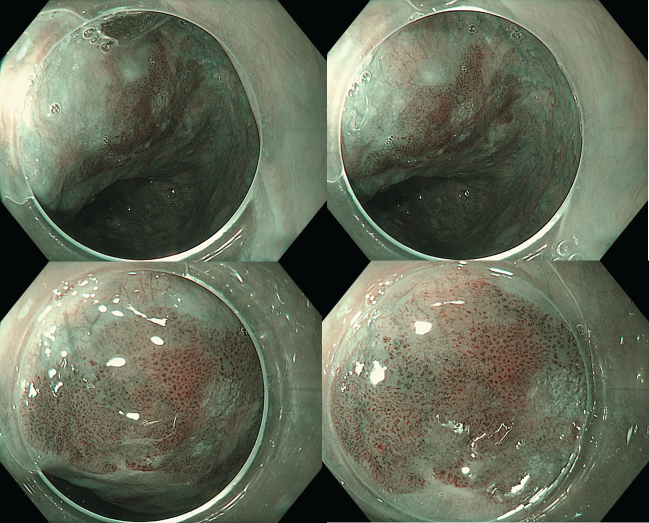
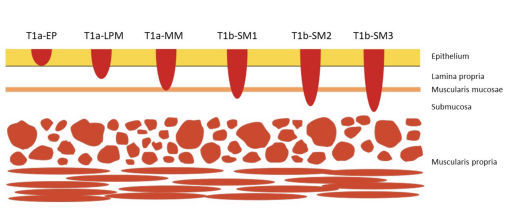
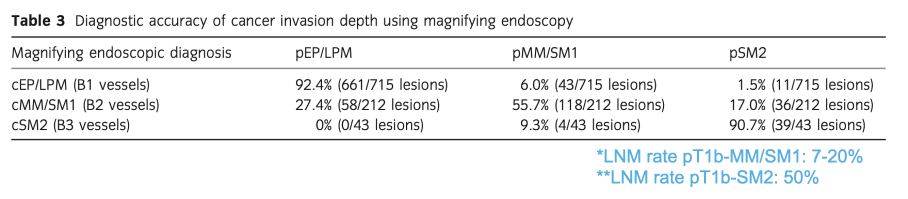
Under NBI observation, the lesion appeared darker brown compared to the surrounding mucosa, showing a positive brownish color (BC+). The lesion’s margins were clearly demarcated. According to the JES classification, microvascular pattern type B1—characterized by fine, loop-like vessels—was identified, suggesting a superficial lesion (T1a-EP/LPM).
Recurrent or New Lesion?
Given the patient’s history, the key question is whether the newly detected lesion represents recurrence or a new (metachronous) cancer.
First, it is essential to differentiate between recurrent and second primary cancers:
Recurrent cancer: occurs when the initial treatment fails to eradicate all cancer cells, leading to regrowth at or near the original site.
Second primary cancer: is a new, independent malignancy that may arise in the same or a different organ. These are classified as:
- Synchronous: detected simultaneously or within 6 months of the initial cancer.
- Metachronous: occurs 6 months or more after the first cancer.
Distinguishing Recurrent Cancer and Metachronous Cancer
| Criteria | Recurrent Cancer | Metachronous Cancer |
| Location | At or near the previous site | Distinct from the previous lesion |
| Scar relation | Often on or near a scarred area | Not related to a scar; surrounding mucosa appears normal |
| Onset | Usually early (within months to 2 years) | May appear early (>6 months) or years later |
| Mechanism | Residual or micrometastatic cancer cells | Field cancerization: mucosal field at risk for new primaries |
| Clinical significance | Requires repeat treatment, often more difficult | Indicates multi-focal cancer risk → requires long-term follow-up |
Based on these criteria, the lesion in this case was determined to be a metachronous esophageal cancer.
Incidence of Second Primary Esophageal Cancer after Surgery
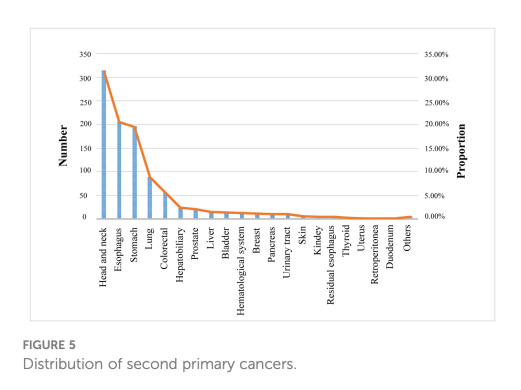
A 2023 meta-analysis by Jie Du et al.
- Reported that the incidence of metachronous esophageal squamous cell carcinoma (MESCC) after endoscopic resection (ER) or surgery is 20.3%, with a cumulative annual risk increase of about 0.2%.
- Second primary cancers after ER or surgery can occur in more than 20 different organs, with the highest frequency in head and neck cancers (31.1%), followed by esophageal cancer (20.5%)
Challenges in Performing ESD
In this case, the diagnosis was metachronous upper-third esophageal cancer in a patient with prior esophagectomy (2024). The depth of invasion was estimated as EP–LPM, and ESD (Endoscopic Submucosal Dissection) was planned.
However, performing ESD posed certain challenges—the lesion was located in the upper esophagus, close to the anastomosis, and the patient had a history of esophageal resection. This increased the risk of reflux reaching the pharyngo-laryngeal area. Therefore, the following precautions were taken:
- Endotracheal intubation if necessary
- Minimal water instillation to reduce reflux
- Shorten procedure time as much as possible
ESD Procedure
- Marking: Dual knife
- Submucosal injection: Non-lifting sign (-)
- Circumferential incision: Dual knife Cut 2 30W
- Submucosal dissection: Dual knife Cut 2 30W + Force coag 30W
- Hemostasis: Soft coag 40W
- ESU: Olympus ESG 100
- Procedure time: 15 minutes
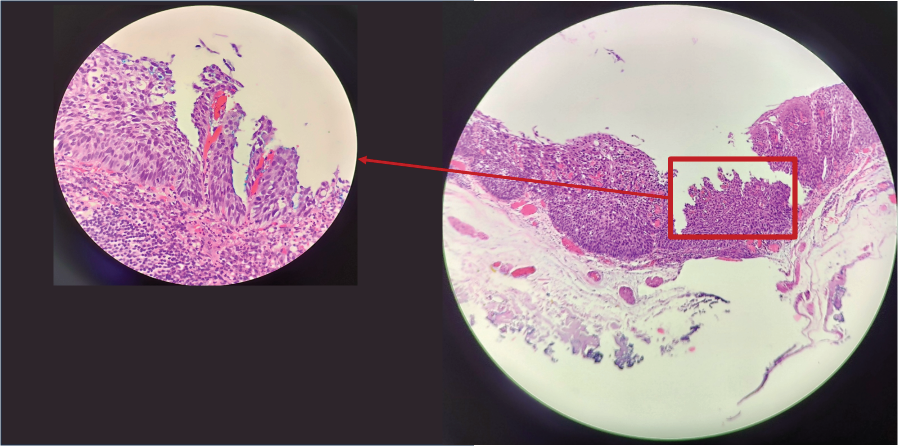
Histopathological Findings after ESD:
- Intraepithelial squamous cell carcinoma
- pTis, v0, ly0, HM0, VM0
- Post-treatment plan: Follow-up
Conclusion
This case highlights an important clinical reality: not all new lesions appearing after esophageal cancer surgery are recurrences. Differentiating between recurrence and metachronous cancer is crucial for accurate diagnosis, prognosis, and management. Additionally, magnifying endoscopy with NBI and JES classification provides an effective tool for assessing invasion depth and selecting a safe, optimal treatment strategy.
Reference:
Du J, et al. Risk factors for metachronous esophageal squamous cell carcinoma after endoscopic or surgical resection of esophageal carcinoma: a systematic review and meta-analysis. Front Oncol. 2023 Sep 14;13:1241572. doi: 10.3389/fonc.2023.1241572.
About ENDOSTORY
ENDOSTORY is a clinical case-sharing series on gastrointestinal endoscopy by Lenus Vietnam, designed to provide valuable insights for endoscopists. Each week, a new “story” is selected and published on Lenus Vietnam’s Facebook fanpage at 8 PM every Friday.
The series is medically supervised by Dr. Tran Duc Canh, an expert in early cancer diagnosis and treatment. Dr. Canh not only performs numerous complex ESD cases but also trains many young endoscopists in Vietnam—helping to popularize this “golden key” technique for early gastrointestinal cancer management. His spirit of sharing and teaching has inspired the creation of this “ENDOSTORY” journey.
For comments or collaboration, please message the Lenus Vietnam fanpage or email [email protected].