[ENDOSTORY #1] When Large Lesions Cross Multiple Mucosal Folds – A Solution from the “Tunneling Method” in Colorectal ESD
In colorectal endoscopy, managing large, widespread lesions—especially those that extend beyond mucosal folds—remains a significant challenge. According to Dr. Trần Cảnh, in such cases, two ESD (Endoscopic Submucosal Dissection) variations can be considered: the Tunneling Method and the Pocket Creation Method (PCM). In the clinical case presented here, the Tunneling Method was applied and successfully used to manage a difficult lesion.
Lesion Approach: Identification and Classification
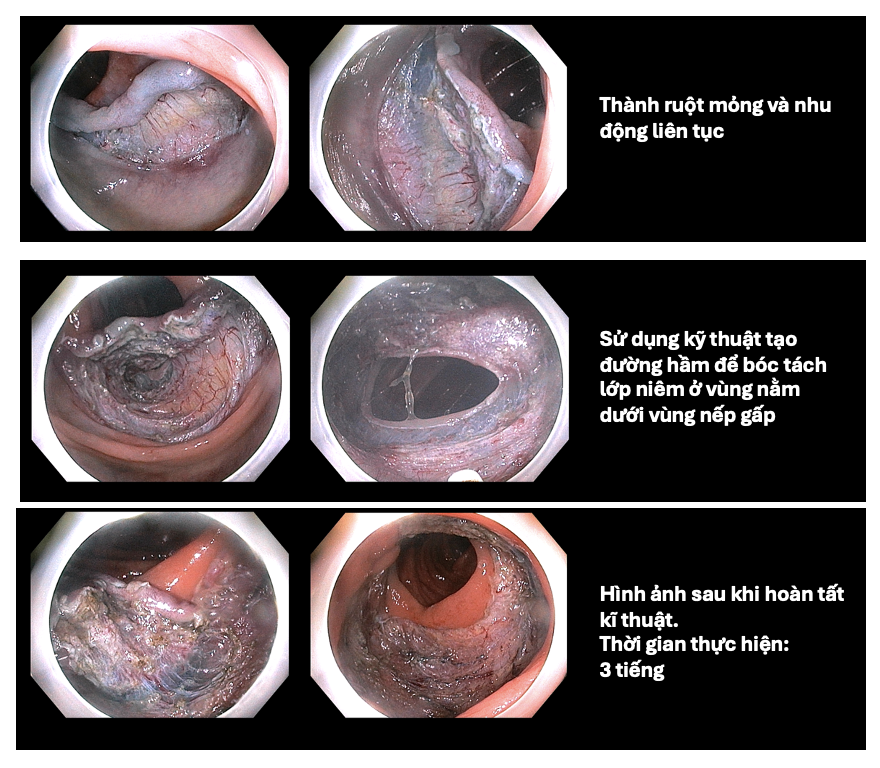
Patient Information: A 68-year-old male presented with digestive disorders and abdominal pain. He had no prior colonoscopy. Upon examination, a flat, widespread lesion was detected in the ascending colon, occupying more than three-quarters of the colon’s circumference and extending over two mucosal folds, making it difficult to observe the entire lesion from a single angle.

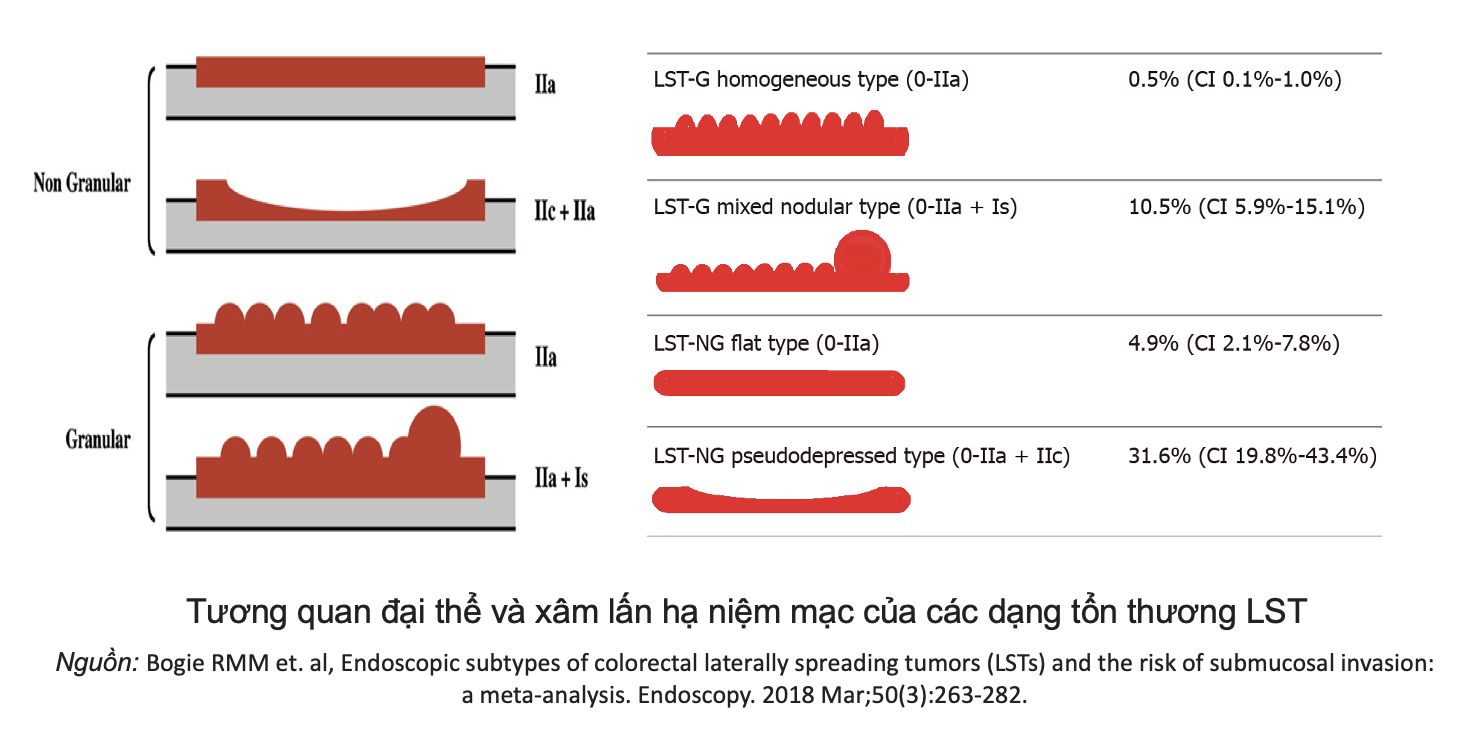
Morphologically, the lesion was consistent with the LST-NG (Laterally Spreading Tumor – Non-Granular) subtype.
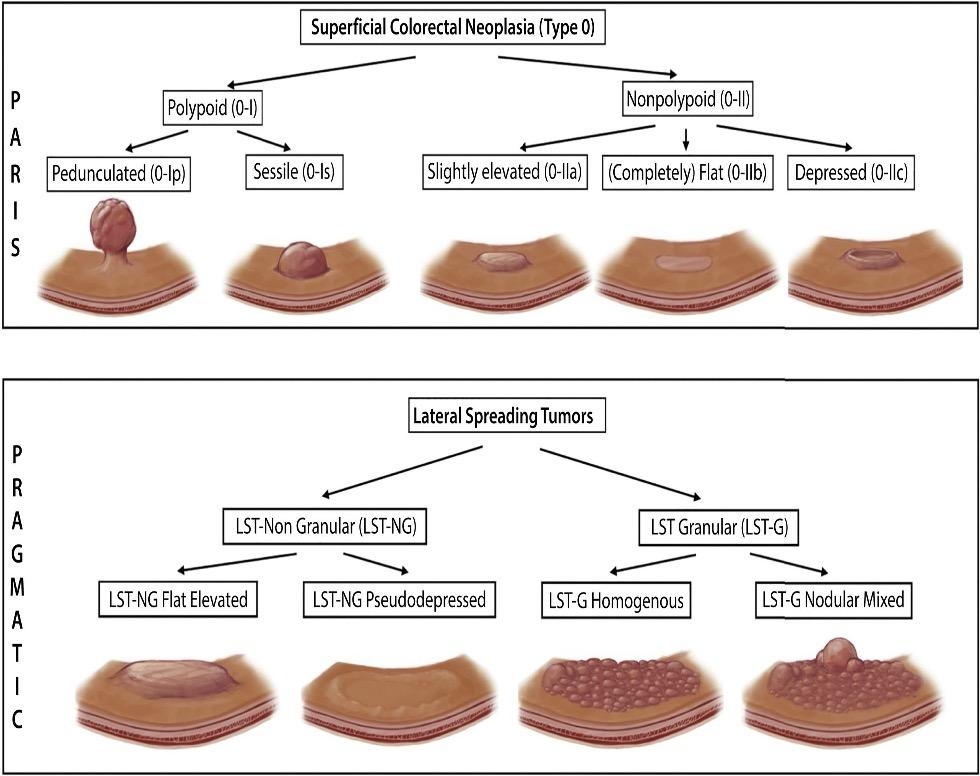
LST (Laterally Spreading Tumor) refers to lesions ≥10mm that grow laterally across the colonic mucosa surface. These lesions are often asymptomatic. LSTs are classified into two main categories:
- LST-G (Granular Type): granular appearance; may be homogeneous or nodular mixed type.
- LST-NG (Non-Granular Type): non-granular, including flat and pseudo-depressed subtypes.
According to a meta-analysis by Bogie, these morphological characteristics are associated with submucosal invasion risk. Specifically, non-granular lesions with pseudo-depression or granular lesions with nodules carry higher risks of submucosal invasion—31% and 10.5%, respectively.
Invasion Risk Assessment: The Role of NBI and JNET Classification
To evaluate the lesion’s invasive potential, the lesion was assessed using Narrow Band Imaging (NBI). It was classified as JNET Type 2A, with evenly distributed, small, homogeneous microvascular structures—suggesting a benign adenomatous lesion confined to the mucosa, with low risk of deep invasion.
The JNET Classification is a useful tool for risk stratification:
- Type 1: commonly seen in hyperplastic polyps, low risk.
- Type 2A: low-grade adenoma, mucosal.
- Types 2B and 3: higher malignancy risk, suspect deep invasion → often require surgical resection.
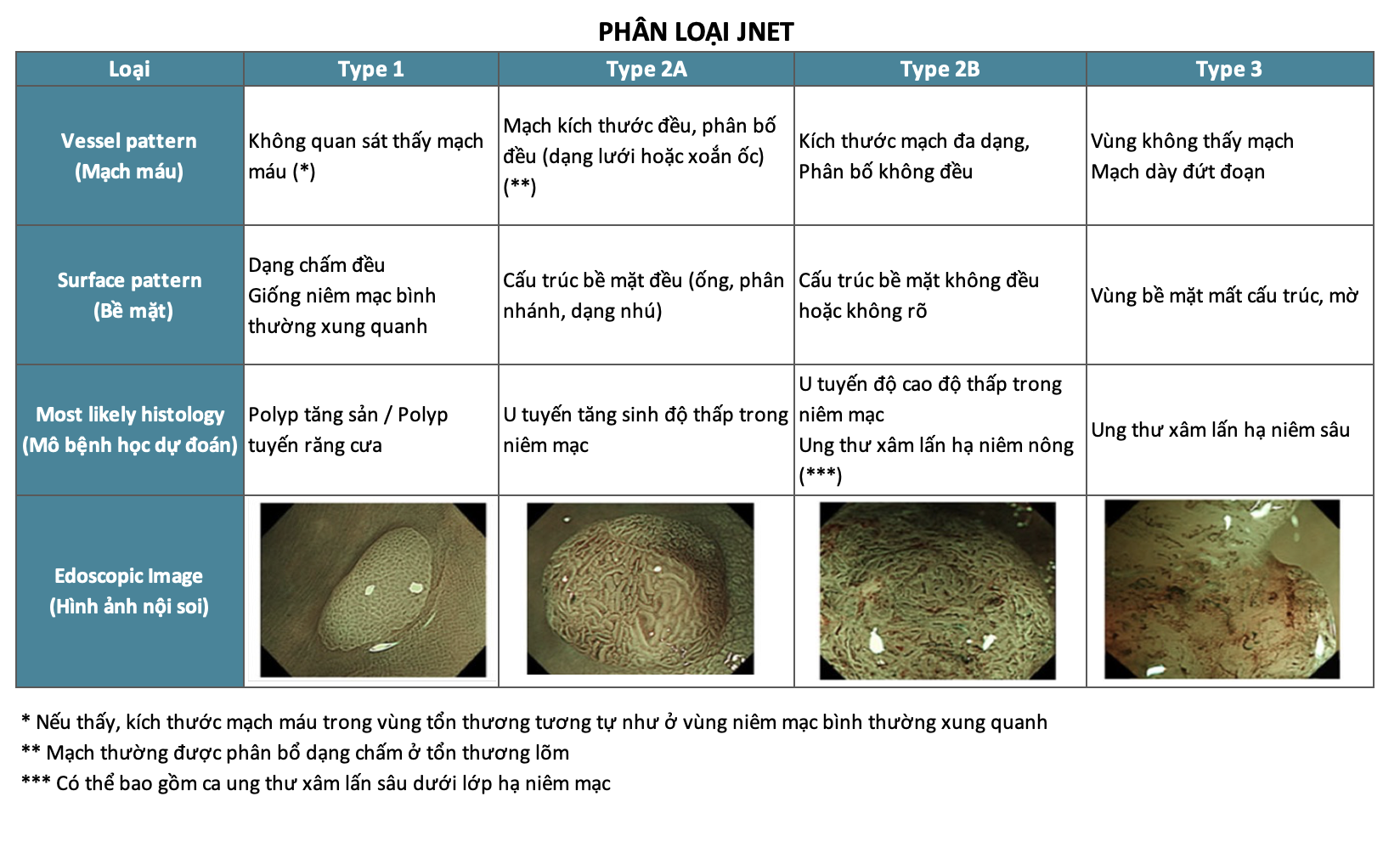
For Type 2A lesions, endoscopic treatment is feasible if the lesion can be safely and completely resected.
Choosing the Appropriate Intervention
The lesion’s size (>20mm), extension across folds, thin mucosa, and adherence to underlying tissue made EMR (Endoscopic Mucosal Resection) challenging and increased the risk of incomplete resection.
ESD was selected as the most appropriate approach due to its capability for en bloc resection and precise margin evaluation. However, due to the lesion’s position and complexity, a more stable approach was needed. Two options were considered: Pocket Creation Method (PCM) and Tunneling Method. The latter was chosen.
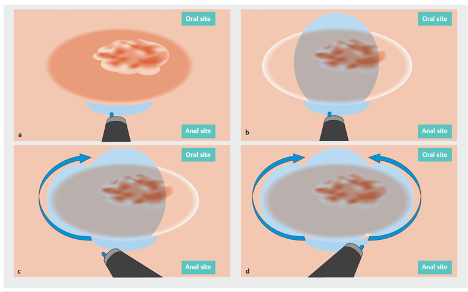
The Tunneling Method
The Tunneling Method involves creating a submucosal tunnel to approach the lesion from beneath, offering better control and stability. Key Steps:
- Incise the mucosa at the distal (oral) and proximal (anal) ends.
- Create a tunnel by dissecting the submucosa from proximal to distal under the lesion.
- After the tunnel is complete, resect the remaining mucosal perimeter around the lesion.
- Complete submucosal dissection to remove the entire lesion en bloc for histopathology.
Advantages:
- Maintained orientation: The tunnel allows stable visualization without obstruction by folds or large lesions.
- Improved vascular control: Enables proactive identification and coagulation of large vessels, reducing bleeding risk and improving safety.
- Suitable for large/wide lesions: Facilitates complete dissection without fragmenting the lesion, minimizing the risk of residual tissue.
Outcome: The procedure was successfully completed in 3 hours.
Conclusion
This case exemplifies the effective use of the Tunneling Method to manage a challenging LST-NG lesion that was large, extended across folds, and located in a hidden area. Careful clinical observation, NBI assessment using the JNET classification, understanding of LST subtypes, and a strategic ESD technique ensured optimal safety and treatment success.
References:
- Bogie RMM et al. Endoscopic subtypes of colorectal laterally spreading tumors (LSTs) and the risk of submucosal invasion: a meta-analysis. Endoscopy. 2018 Mar;50(3):263-282.
- Kudo SE et al. Flat and depressed types of early colorectal cancers: from East to West. Gastrointest Endosc Clin N Am. 2008 Jul;18(3):581-93, xi.
- Fukuzawa M et al. History of endoscopic submucosal dissection and role for colorectal endoscopic submucosal dissection: A Japanese perspective. Gastrointestinal Intervention. 2012;1(1):30-35.
About the ENDOSTORY Series
ENDOSTORY is a clinical case-sharing series on gastrointestinal endoscopy curated by Lenus Vietnam, aiming to provide practical, insightful content for endoscopists. Each week, one case story is selected and posted on the Lenus Vietnam fanpage every Friday at 8 PM.
The series is medically advised by Dr. Trần Cảnh, a leading expert in early cancer detection and treatment. Not only is he involved in complex ESD procedures, but he also trains many young Vietnamese endoscopists in ESD—a technique often seen as the “golden key” for early GI cancer treatment. His spirit of sharing inspired the creation of this storytelling journey.
The program is still in its early stages and welcomes feedback for improvement. Please feel free to message the Lenus Vietnam fanpage or email [email protected] with your comments.