Endostory No.15: The post ESD journey: Unexpected complications and management
In interventional endoscopy, sometimes we think the biggest challenge is over once we have completely resected a complex lesion. However, in reality, the post-ESD journey may hold even more surprises than the procedure itself. This week’s case in ENDOSTORY #15 is a clear illustration: a large LST-type lesion in the cecum was successfully managed, but the real complication appeared in the days following the intervention.
Case introduction
A 71-year-old male patient, previously healthy, was found to have multiple colorectal polyps during a screening endoscopy at a lower-level hospital and was referred to an upper-level hospital for further evaluation.
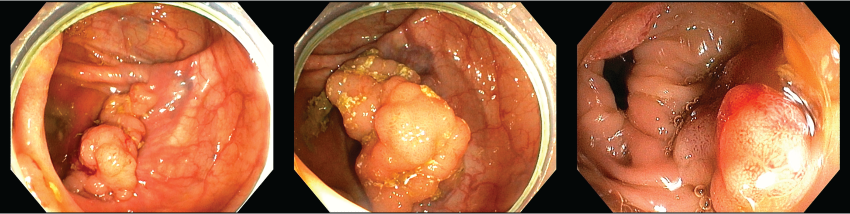
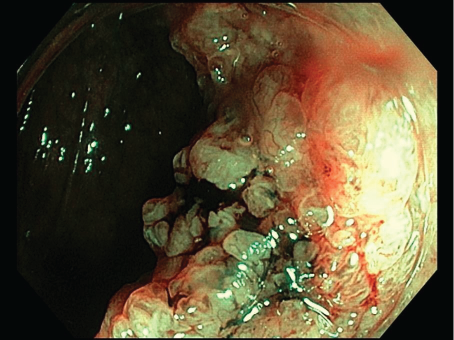
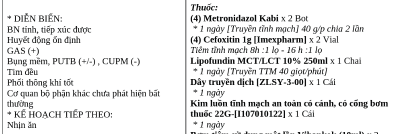
During endoscopy, the physician detected an LST-G nodular mixed lesion measuring about 50 mm at the cecum, on the background of multiple colonic polyps. Endoscopy with NBI showed glandular and villous surface epithelial structures with relatively homogeneous vascular patterns, no significant dilation, abundant mucus and exudates, and was evaluated as JNET Type 2A.
The cecum, in endoscopy, is considered a particularly difficult location because the maneuverability of the scope is limited. In addition, the bowel wall here is thinner, with more fat than other sites; if the lesion is located at the base of the cecum, the muscular layer is vertical, requiring great caution. Moreover, as the cecum is the deepest part of the colon, delayed complications such as perforation or bleeding are more difficult to manage conservatively. Therefore, when deciding to perform ESD at this location, physicians must take into account:
- Possible difficulties with scope maneuverability
- Determining the relation to the appendiceal orifice and ileocecal valve
- Optimizing dissection using gravity
- Considering traction in case of difficulty
ESD intervention
In this case, the physician prioritized treating the lesion at the cecum first. Due to the anticipated difficulty of the location and prolonged procedure time, the remaining polyps would be treated in a later session.
The procedure lasted 100 minutes, and the patient underwent successful ESD without intra-procedural complications.
The post-ESD journey – the most stressful days
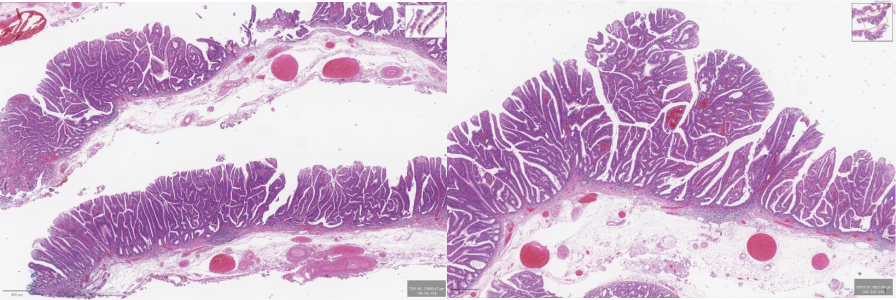
On Day 1, the patient was alert, afebrile, with no abdominal pain, and had a soft abdomen on examination. However, due to advanced age, large lesion size, and cecal location, the patient was considered at high risk of delayed complications and was closely monitored. He was placed on complete fasting, IV fluids, parenteral nutrition, and prophylactic antibiotics.
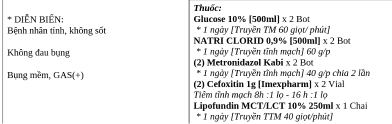
On Day 2, the patient developed right lower abdominal pain (intervention site), mild fever (37.5°C), and abdominal distension (GAS+). Abdominal examination still revealed a soft abdomen with no clear peritoneal signs. This was a clinically difficult moment – differentiation between delayed perforation and post-ESD coagulation syndrome (PECS) was required.
Post-ESD coagulation syndrome (PECS) is a localized peritonitis condition with abdominal pain, fever, and elevated inflammatory response; most cases can be managed symptomatically. Currently, risk factors and preventive measures remain unclear, and sometimes it is difficult to differentiate from delayed perforation. The important point is to perform imaging when needed and not miss cases requiring surgery.
Risk factors for PECS include: female gender, lesion location at the ascending colon and cecum (1)(2), lesion size ≥40 mm, and procedure time ≥90 minutes.
The team decided to perform an urgent abdominal X-ray. Results showed no subdiaphragmatic free air, excluding perforation; but with localized pain and 3/4 risk factors (cecal location, lesion ≥40 mm, procedure ≥90 minutes), the diagnosis was directed towards PECS. The patient continued to receive conservative management: fasting, antibiotics, parenteral nutrition, and close monitoring.

On Day 3, the patient only had localized tenderness, no fever, and was able to resume oral intake in the evening.
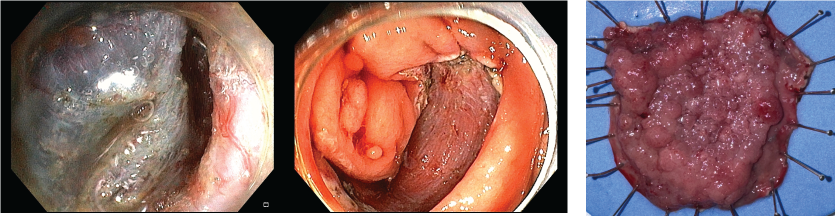
On Day 4, the patient no longer had abdominal pain or fever, passed yellow stools, but with small clots (considered residual blood from intervention). By evening, however, he passed dark stools with multiple clots and fresh blood, raising suspicion of delayed post-ESD bleeding.
Vital signs (pulse, temperature, blood pressure) and CBC showed stable hemodynamics and only a mild Hb decrease within follow-up range. However, due to multiple risk factors, the physician decided to perform urgent endoscopy for hemostasis.
Surprising result: the cecal ESD site was stable, with no active bleeding. The true source of bleeding was a large untreated polyp in the sigmoid colon. With patient and family consent, the team performed polypectomy using an endoloop, both treating and definitively resolving the bleeding cause.
Afterwards, the patient resumed oral intake on Day 5 noon. The team decided on early feeding after assessing stable general condition, as prolonged fasting may affect ulcer healing.
On Day 6, the patient was stable, with no abdominal pain or rectal bleeding, and was discharged the following day.
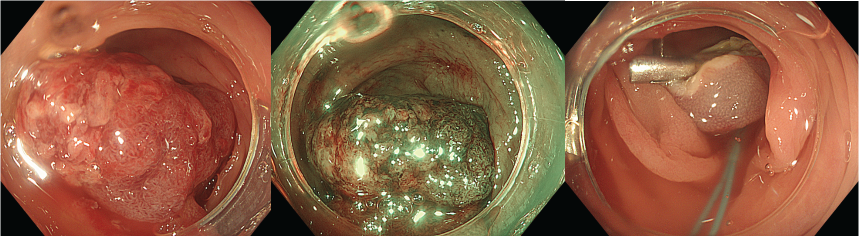
Histopathology
Histopathology showed a tubulovillous adenoma with high-grade dysplasia. Importantly, both deep and lateral margins were negative, confirming complete resection with no residual tumor cells at the margins. This validated that despite multiple post-procedure complications, from the technical standpoint, this was a successful ESD – completely removing a precancerous lesion with malignant potential.
Conclusion
- Cecal ESD can be performed safely with thorough preparation but always carries the risk of PECS and delayed complications.
- Post-ESD monitoring is a critical phase, requiring daily close evaluation to differentiate delayed perforation from coagulation syndrome and detect early bleeding.
- In patients with multiple colonic polyps, complications may arise not from the main ESD site but from untreated lesions.
- Urgent endoscopy is not only for temporary hemostasis but also an opportunity to definitively treat high-risk polyps, reducing recurrence and future complications.
References in this article:
(1) Jung D, Youn YH, Jahng J et al. Risk of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Endoscopy 2013; 45: 714–717.
(2) Choo WK, Subhani J. Complication rates of colonic polypectomy in relation to polyp characteristics and techniques: a district hospital experience. J Interv Gastroenterol 2012; 2: 8–11.
About ENDOSTORY
ENDOSTORY is a clinical case-sharing series on gastrointestinal endoscopy, carried out by Lenus Vietnam, aiming to provide useful information for endoscopists. Each week, one “story” is carefully selected and posted on Lenus Vietnam’s fanpage at 8:00 PM every Friday.
The series is medically supervised by Dr. Trần Đức Cảnh – an expert in the diagnosis and treatment of early cancer. Not only has he directly participated in numerous complex ESD cases, but Dr. Trần Đức Cảnh is also a mentor who has trained many young endoscopists in Vietnam, contributing to the widespread adoption of ESD – regarded as the “golden key” in early GI cancer treatment. His spirit of sharing and dedication is one of the inspirations behind the ENDOSTORY journey of “telling endoscopic stories.”
For feedback or discussion, please inbox Lenus Vietnam’s fanpage or email us at [email protected] so we can listen to you.